| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://www.neurores.org |
Original Article
Volume 13, Number 1, September 2023, pages 33-42
Seasonal Variation in Ischemic Stroke Hospitalization: Results From a Large Health System in Six Western States of the United States
Reza Bavarsad Shahripoura, b, j, Datis Azarpazhoohc, Elizabeth Baraband, Horia Margineane, Sima Osouli Meinaghf, Sholeh Faezig, Jasen Tarpleyh, i
aDepartment of Neurology, Comprehensive Stroke Center, Loma Linda University, Loma Linda, CA, USA
bComprehensive Stroke Center, University of California San Diego (UCSD), San Diego, CA, USA
cDepartment of Medical Sciences, University of Western Ontario, London, ON, Canada
dProvidence Saint John’s Health Center, Neurovascular and Stroke Center, Santa Monica, CA, USA
eProvidence Brain and Spine Institute, Providence St Joseph Health, Portland, OR, USA
fDepartment of Neurology, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
gDepartment of Clinical Neurological Sciences, University of Western Ontario, London, ON, Canada
hProvidence St Johns Health Science Center, Santa Monica, CA
iDepartment of Neurology, Pacific Neuroscience Institute, Santa Monica, CA, USA
jCorresponding Author: Reza Bavarsad Shahripour, Department of Neurology, Comprehensive Stroke Center, Loma Linda University, Loma Linda, CA, USA
Manuscript submitted December 14, 2022, accepted June 7, 2023, published online August 8, 2023
Short title: Seasons and Stroke
doi: https://doi.org/10.14740/jnr745
| Abstract | ▴Top |
Background: Evidence of seasonal variations in the number of stroke admission is inconsistent with some studies reporting no association and some a significant rise in different months of the year. In addition, less is known about how seasonality impacts the admission according to stroke subtype.
Methods: This was a cross-sectional, observational study of data from a hospital-based registry (n = 40 hospitals) affiliated with Providence Health and Services in Alaska, California, Montana, Oregon, Texas, and Washington state. We included all cases with acute ischemic stroke admitted from March 1, 2017, to February 29, 2020. Admission data were categorized according to four meteorological seasons: winter, spring, summer, and fall. Acute ischemic stroke was categorized into two sub-types as large vessel occlusion (LVO) or non-LVO. We calculated the aggregate number of individuals admitted with stroke by season. Using linear regression models with generalized estimating equations (GEEs), we assessed the relationship between meteorological season and daily hospitalization number. We used R version 4.0.4 (2021-02-15) for both the descriptive and inferential analyses and the R gee pack package (version 1.2-1) to perform GEEs.
Results: During the study period, we identified 18,886 patients with acute ischemic stroke (median age: 73; 48.7% women). Acute ischemic stroke was more commonly observed during winter compared with other seasons with some variations between the selected regions. Based on a GEE model, stroke hospitalization increased during winter, with an additional 3.3 cases per day in comparison with spring in the whole population (beta: 3.3, 95% confidence interval (CI): (2.4, 4.1), P < 0001). Winter is also associated with a higher number of LVO.
Conclusions: The total number of ischemic stroke admissions, including cases of LVO, increased during the winter months. The results are important for human resource allocation for better management of cases with ischemic strokes.
Keywords: Ischemic stroke; Incidence; Hospitalization; Season; Stroke subtypes; Etiology; Large vessel occlusion
| Introduction | ▴Top |
Evidence of seasonal changes in the incidence of stroke is inconsistent. While some studies showed no association between seasons and strokes [1], hospitalization rate in most studies peaked in different seasons including, spring [2], summer [3], autumn [4, 5], and winter [6, 7]. These variations in findings can be explained partially by the different sample sizes [8], study design (hospital vs. population-based) [2], short observation periods [8], statistical model for data analysis, regional vs. national data selection [9], and geographical location of the study population [3]. In addition, less is known about how seasonality impacts the incidence of stroke subtype [10].
With recent advances in hyper-acute stroke care including thrombolytic and endovascular therapy, we hope the data help hospitals to identify seasons with the highest number of stroke codes and admissions. Also, it may help and guide human resources for a more time-based approach in the future.
The current study was designed to identify seasonal changes in the number of stroke hospitalization and stroke subtype in the western USA.
| Materials and Methods | ▴Top |
Ethics
This study was approved by the Institutional Review Board of Providence Health and Services with a waiver of informed consent. We followed the reporting guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement for observational studies [11].
Setting
This was a cross-sectional study of data from a hospital-based registry focused on improving care for patients diagnosed with a stroke. Data were collected for clinical care and quality improvement by 40 hospitals affiliated with Providence Health and Services. Providence Health System is a large healthcare system located in Alaska, California, Montana, Oregon, Texas, and Washington. All adult inpatients with a diagnosis of acute ischemic stroke at admission within Providence Health and Services from March 1, 2017, to February 29, 2020, were included.
We excluded patients younger than 18 years old, where target lesion was not recorded, patients who were diagnosed with a transient ischemic attack (TIA), and patients with stroke mimics. Exploratory data analysis was carried out before formal analysis through inspection of graphical data of the hospitalization of acute ischemic stroke over time for each hospital. We excluded patients from sites that showed inconsistent data collection reflected in scattered missing data. We also excluded patients from sites with small stroke patient volume (averaged fewer than 60 patients per year). In addition, we excluded cases from time periods and sites where annual data collection was incomplete or where data for full seasons were not available. In clinical registries, there is a recognized time lag between the event occurrence and data entry [12]. As a result, our final analytic cohort represents cases admitted for stroke from March 1, 2017, to February 29, 2020.
Study variables and definitions
Ischemic stroke was defined according to the updated definition of stroke for the 21st century [13]. Acute ischemic stroke was categorized into two sub-types as large vessel occlusion (LVO) or non-LVO. LVO was identified based on the clinical history of acute ischemic stroke and neurovascular imaging findings. We classified our centers based on their stroke center certification status into primary stroke centers, comprehensive stroke centers, thrombectomy-capable stroke centers, and centers without any certification.
The daily number of acute ischemic stroke admissions was calculated from the date of patient arrival at the hospital. Admission data were categorized according to four meteorological seasons. Winter was defined as December 1, to February 28 (29 in a leap year), spring from March 1, to May 31, summer from June 1, to August 31, and fall from September 1, to November 30. We selected the meteorological season classification because it is based on seasonal temperature patterns. Since the western USA includes states with diverse regional climates ranging from subarctic to warm desert climates, we made a commonsense judgment about weather patterns and grouped states into three regions accordingly: 1) Alaska; 2) California and Texas; and 3) Montana, Washington, and Oregon. In this exploratory analysis, we included well-recognized risk factors for acute ischemic stroke: demographic (age at arrival, sex, and race), and comorbidity (hypertension, dyslipidemia, atrial fibrillation or flutter, previous stroke, diabetes mellitus, obesity).
Statistical analysis
Baseline characteristics and comorbidities were described by season. Categorical variables were described using percentages. Continuous variables were summarized using medians and interquartile ranges. Differences in these characteristics were compared using Pearson’s Chi-squared test or Fisher’s exact test where appropriate for categorical variables and Wilcoxon’s matched pairs test and paired t-tests for continuous variables.
Our primary outcome was the aggregate number of individuals admitted with acute ischemic stroke by season. Linear regression models with generalized estimating equations (GEEs) were used to model the relationship between meteorological season and daily presentation with acute ischemic stroke. GEE allowed us to account for the repeated measurement of stroke hospitalization over time. The daily number of stroke admissions was set as the dependent variable in the model. Demographic, region, stroke center certification status, and comorbidities defined above were included as the independent variables. An exchangeable working correlation structure was selected based on the quasi-likelihood under the independence model criterion.
We used GEE to report increase or decrease on daily admission number of stroke patients according to different seasons. All differences are reported based on adjusted beta after controlling the effect of possible risk factors.
We selected GEE as this model can represent changes in number of admissions. This is an appropriate model for our data analysis as our data have a normal pattern of distribution. In addition, clinicians and administrative authorities in hospitals can understand easily changes in number based on season and allocate their resources accordingly. The clinical outcome was the estimated day change in average acute ischemic stroke occurrence when progressing from one season to another.
Our secondary outcome was the number of ischemic stroke admission stratified according to LVO. For our subgroup analysis of stroke subtype based on the presence of vessel occlusion, we only considered patients with the time of onset to admission within 24 h. The objective of this analysis was to identify seasonal variation in the number of treatment-eligible stroke patients with thrombolytic therapy or endovascular treatment, as these patients represent the greatest healthcare resource utilization. To this end, we excluded cases that were admitted to the hospital more than 24 h after the last known-well time because these patients are typically ineligible for revascularization therapy.
Regression coefficient estimates and 95% confidence intervals (CIs) are reported. Two-tailed P values were reported, and P values less than 0.05 were considered significant. R version 4.0.4 (2021-02-15) was used for both the descriptive and inferential analyses. The GEEs were run using the R gee pack package (version 1.2-1).
| Results | ▴Top |
The registry enrolled 138,836 patients of which 119,950 were excluded from the analysis. Our analytic sample consisted of 18,886 patients with acute ischemic stroke who were admitted over a 3-year period (Fig. 1). The demographic and clinical characteristics of our cohort are shown in Table 1. We estimated the seasonality in the overall ischemic cohort (n = 18,886) and separately for each of the two subtypes, LVO (n = 4,382) and non-LVO (n = 9,571).
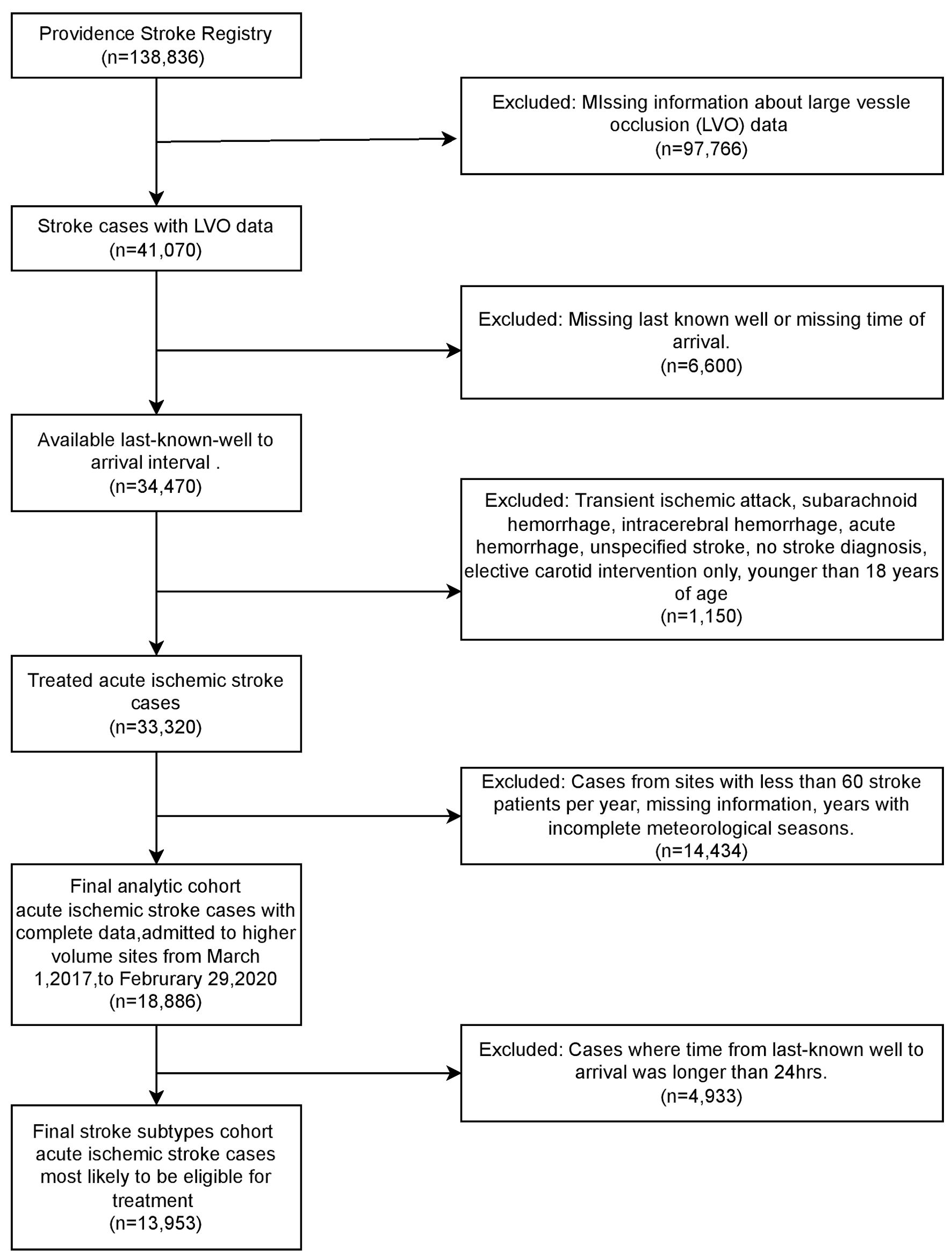 Click for large image | Figure 1. Flow chart of cohort selection. LVO: large vessel occlusion. |
 Click to view | Table 1. Patient Characteristics by the Season of Admission for Ischemic Stroke |
Seasonality of acute ischemic stroke
Overall, the seasonal pattern of acute ischemic stroke over the 3-year analysis period in the western USA shows a steady increase in the number of stroke hospitalization (Fig. 2).
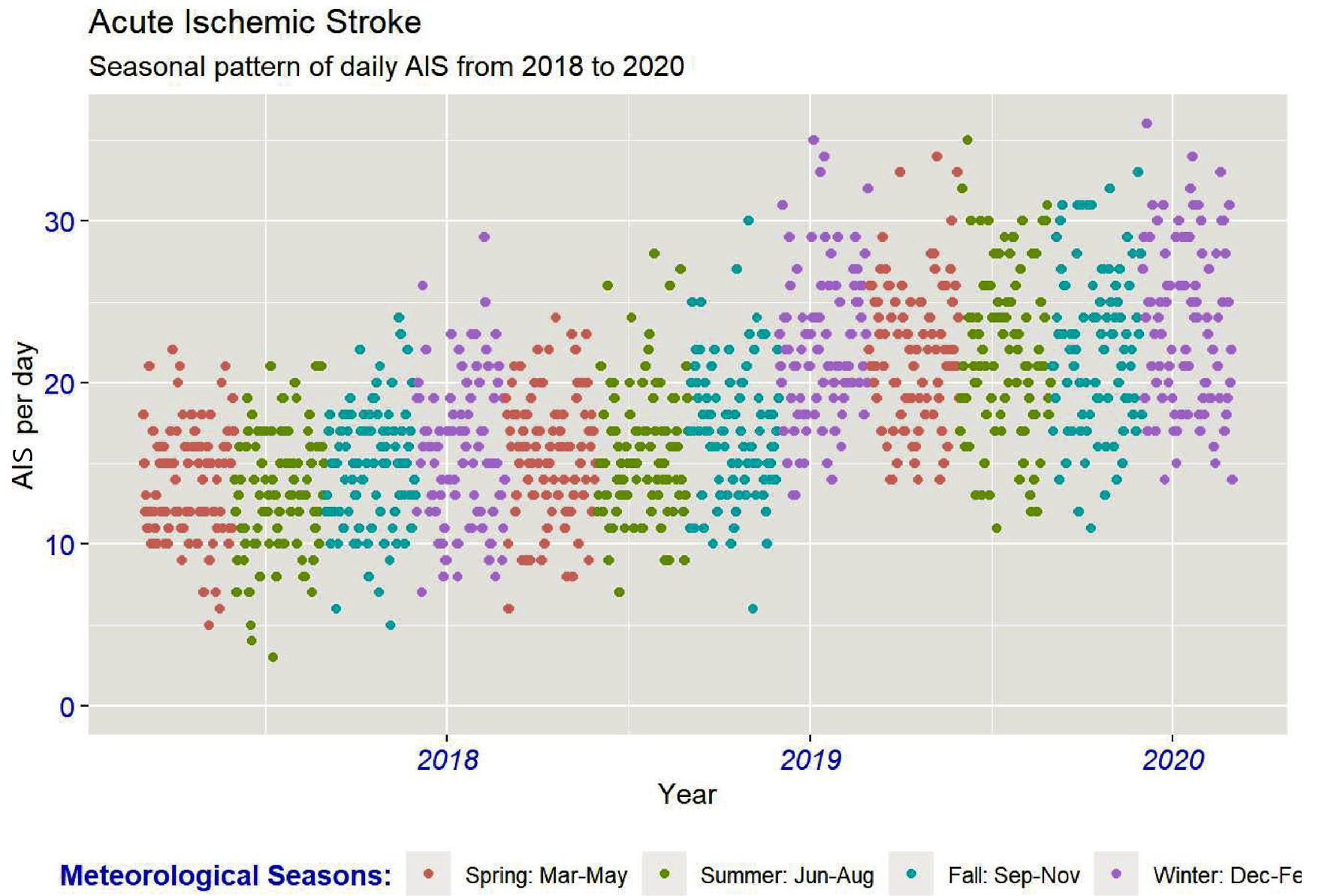 Click for large image | Figure 2. Seasonal pattern of daily acute ischemic stroke hospitalization in six western states of the USA. AIS: acute ischemic stroke. |
Acute ischemic stroke was more frequent during the winter compared with other seasons (spring 4,565 (24.2%), summer 4,482 (23.7%), fall 4,692 (24.8%), winter 5,147 (27.3%)) (Table 1). There were differences in the hospitalization of stroke between seasons by region. In Alaska, the season with the highest number of strokes was summer (n = 275) (Table 1). In contrast, winter was the season with the highest number of strokes for the region of California and Texas (n = 2,361) and the region of Montana, Washington, and Oregon (n = 2,573) (Table 1). The relative distribution of strokes between regions also differed by season. In Alaska, the season with the highest relative frequency of stroke was summer, with 6.1% of all strokes occurring during the summer admitted to sites in Alaska. In the region of Montana, Washington, and Oregon, spring was the season with the highest relative frequency of stroke, with 54.7% (n = 2,499) of all strokes occurring during spring admitted to sites in this region. In California and Texas, winter had the highest relative frequency of strokes, with 45.9% (n = 2,361) of strokes occurring during winter admitted to sites in California and Texas (P value < 0.0001) (Table 1). Patient demographics and clinical characteristics were balanced between seasons.
We next investigated the seasonal variation of ischemic stroke, using the GEE model with acute ischemic stroke as the response variable. As Figure 2 demonstrates the average daily admission of acute ischemic stroke from 2018 to 2020, which is around 15 - 25 events per day, using the beta coefficient test and adjusting based on stroke risk factors revealed the most significant increase in daily admission of acute ischemic stroke between spring and winter, which was 3.3 more cases per day.
The results indicate that there were strong seasonal patterns of acute ischemic stroke admissions (Table 2). In the unadjusted model, the total admission per day of acute ischemic stroke increased by about one case per day between spring and fall (95% CI: (0.05, 1.6), P value = 0.04) (Table 2), and by 3.6 cases per day between spring and winter (95% CI: (2.7, 4.4), P value < 0.001) (Table 2). After controlling for stroke risk factors, there was no significant difference in the number of admissions between spring and fall (beta: 0.66, 95% CI: (-0.14, 1.5), P value = 0.10) (Table 2). However, between spring and winter, the daily admission of acute ischemic stroke increased (beta: 3.3 patients per day; 95% CI: (2.4, 4.1), P value < 0.001).
 Click to view | Table 2. Estimation Results From the Generalized Estimating Equations (GEE) Model, the Association of Season With the Number of Acute Ischemic Stroke Admission |
In sequential comparisons between seasons using the multivariate GEE model, no significant relationships were observed between spring and summer (slope: -0.1; 95% CI: (-0.9, 0.7), P value < 0.8) nor between summer and fall (slope: -0.1; 95% CI: (-0.1, 1.6), P = 0.08). However, between fall and winter, the total admission per day in acute ischemic stroke increased by 2.6 patients per day (95% CI: (1.7, 3.5), P value < 0.001).
We next examined seasonal admission of stroke by ischemic stroke subtypes, i.e., LVOs vs. those without LVO. Similar to the whole cohort, the number of admitted cases with LVO was lower in the spring and summer, increased in fall, and highest during the winter (Table 3).
 Click to view | Table 3. Estimation Results From the Generalized Estimating Equations (GEE) Model, the Association of Season With the Number of Acute Ischemic Stroke Subtypes Admission |
| Discussion | ▴Top |
Our study has important clinical applications for stroke centers. In a large data of 18,886 patients with acute ischemic stroke in six states of the USA, we found a significant variation in the number of stroke hospitalization with a higher admission during winter. Likewise, the number of cases with LVO was significantly higher during this period.
Stroke hospitalization rates varied by season in different studies with most of them indicating an association between cold weather and the occurrence of ischemic strokes [6, 14-17]. In the line of these studies, we found a significant rise in the hospitalization of ischemic strokes during wintertime. Higher hospitalization is not the only clinical challenge during cold weather. From the pooled systematic analysis of ambient temperature effect in stroke, older age was more vulnerable to the lower temperature [18]. During colder months, strokes are also likely to be more severe with a higher rate of mortality [15, 16, 19, 20]. Consequently, stroke centers may have more challenges in the management and workflow of cases with stroke during this period of time.
With recent advances in endovascular therapy, it is crucial to identify any possible changes in the incidence of LVO in stroke centers. The current evidence regarding LVO hospitalization according to season/month is scarce. In a Japanese study (n = 12,660, between May 1999 and April 2000), cardioembolic stroke was more frequent during wintertime [21]. Likewise, another Japanese study revealed a higher incidence of hemorrhagic stroke and cardioembolic stroke in winter and non-cardioembolic strokes in summer [22]. In a hospital-based study (n = 2,628), Bucke et al noticed more mechanical thrombectomy in spring and early autumn [23]. In our study, we found a higher number of LVO during winter.
There are many hypotheses about the risk factors of ischemic stroke in cold months. Atrial fibrillation, which is an important risk factor for ischemic stroke especially LVO, is reported more frequent in colder months because of higher rate of hypertension, symptomatic activation, and higher platelet count and blood viscosity in lower temperatures [24-26]. In our study, atrial fibrillation rate did not show a significant difference between seasons nor between the LVO and non-LVO groups.
Influenza and influenza like symptoms are another hypothesis on the increased risk of cardiovascular events in winter [27]. Kulick et al reported higher rate of ischemic stroke after influenza like illnesses, which is more common in cold weather, especially in men and people living in rural areas [28].
Air pollution as another meteorological factor can although affect the incidence of stroke. In a systematic review, admission to hospital or mortality from stroke was associated with increased level of gaseous pollutants and particulate matters especially on the exposure day [29]. These findings were confirmed with another more recent meta-analysis which has reported positive association of all six air pollutants and stroke hospital admission [30].
Our study has some limitations. There was missing information about LVO data in the majority population of the providence health registry and we have excluded them from our analysis. We do not have access to the severity of stroke at admission and therefore we cannot comment on the difference in stroke severity based on the season. The occurrence of coronavirus disease 2019 (COVID-19) may affect the hospitalization rates since the pandemic [31]. Despite an overall decline in the stroke hospitalization after the pandemic, the pattern of hospitalization based on season remained stable with a higher number of admissions in winter even during the pandemic. We have access to hospital-based information which is not representative of our community. Patients admitted to the hospital are more likely to have severe stroke with LVO as compared to lacunar strokes. However, this is a systematic limitation across all provinces/seasons and may not affect our final findings. Our major strength is having access to large data from 40 hospitals in the USA, which provides an opportunity to perform the current study and follow changes in hospitalization in detail.
In summary, we found that the number of stroke hospitalization increased over time overall, with a higher admission number peaking annually during the winter months. Because effective stroke treatment is a race against time, it is crucial for healthcare systems to identify seasons with the highest number of admissions. This information will provide a rational approach for human resource allocation, will help avoid staff burnout, and may lead to better stroke outcomes for patients.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Authors Contributions
Reza Bavarsad Shahripour: study design, writing the first draft. Datis Azarpazhooh: revising the manuscript. Elizabeth Baraban: data collection. Horia Marginean: data analysis. Sima Osouli: literature review, revising the manuscript. Sholeh Faezi: revising the manuscript. Jasen Tarpley: study design.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
AIS: acute ischemic stroke; TIA: transient ischemic attack; CIs: confidence intervals; LVO: large vessel occlusion; IQR: interquartile range; AF: atrial fibrillation; GEE: generalized estimating equation; B: beta confident; STROBE: Strengthening the Reporting of Observational Studies in Epidemiology
| References | ▴Top |
- Skajaa N, Horvath-Puho E, Sundboll J, Adelborg K, Rothman KJ, Sorensen HT. Forty-year seasonality trends in occurrence of myocardial infarction, ischemic stroke, and hemorrhagic stroke. Epidemiology. 2018;29(6):777-783.
doi pubmed - Karagiannis A, Tziomalos K, Mikhailidis DP, Semertzidis P, Kountana E, Kakafika AI, Pagourelias ED, et al. Seasonal variation in the occurrence of stroke in Northern Greece: a 10 year study in 8204 patients. Neurol Res. 2010;32(3):326-331.
doi pubmed - Salam A, Kamran S, Bibi R, Korashy HM, Parray A, Mannai AA, Ansari AA, et al. Meteorological factors and seasonal stroke rates: a four-year comprehensive study. J Stroke Cerebrovasc Dis. 2019;28(8):2324-2331.
doi pubmed - Sipila JO, Ruuskanen JO, Kauko T, Rautava P, Kyto V. Seasonality of stroke in Finland. Ann Med. 2017;49(4):310-318.
doi pubmed - Jin H, Xu Z, Li Y, Xu J, Shan H, Feng X, Xie Y, et al. Seasonal variation of stroke incidence in Wujin, a city in southeast China. Health Sci Rep. 2018;1(4):e29.
doi pubmed pmc - Diaz A, Gerschcovich ER, Diaz AA, Antia F, Gonorazky S. Seasonal variation and trends in stroke hospitalizations and mortality in a South American community hospital. J Stroke Cerebrovasc Dis. 2013;22(7):e66-69.
doi pubmed - Liao JN, Chao TF, Liu CJ, Chen SJ, Hung CL, Lin YJ, Chang SL, et al. Seasonal variation in the risk of ischemic stroke in patients with atrial fibrillation: A nationwide cohort study. Heart Rhythm. 2018;15(11):1611-1616.
doi pubmed - Raj K, Bhatia R, Prasad K, Srivastava MV, Vishnubhatla S, Singh MB. Seasonal differences and circadian variation in stroke occurrence and stroke subtypes. J Stroke Cerebrovasc Dis. 2015;24(1):10-16.
doi pubmed - Oberg AL, Ferguson JA, McIntyre LM, Horner RD. Incidence of stroke and season of the year: evidence of an association. Am J Epidemiol. 2000;152(6):558-564.
doi pubmed - Spengos K, Vemmos KN, Tsivgoulis G, Synetos A, Zakopoulos N, Zis VP, Vassilopoulos D. Seasonal variation of hospital admissions caused by acute stroke in Athens, Greece. J Stroke Cerebrovasc Dis. 2003;12(2):93-96.
doi pubmed - von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85(11):867-872.
doi pubmed pmc - Salemi JL, Tanner JP, Anjohrin SB, Rutkowski RE, Correia JA, Watkins SM, Kirby RS. Evaluating difficult decisions in public health surveillance: striking the right balance between timeliness and completeness. J Registry Manag. 2015;42(2):48-61.
pubmed - Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(7):2064-2089.
doi pubmed - Feigin VL, Nikitin YP. Seasonal variation in the occurrence of ischemic stroke and subarachnoid hemorrhage in Siberia, Russia. A population-based study. Eur J Neurol. 1998;5(1):23-27.
doi pubmed - Lichtman JH, Jones SB, Wang Y, Leifheit-Limson EC, Goldstein LB. Seasonal variation in 30-day mortality after stroke: teaching versus nonteaching hospitals. Stroke. 2013;44(2):531-533.
doi pubmed pmc - Chu SY, Cox M, Fonarow GC, Smith EE, Schwamm L, Bhatt DL, Matsouaka RA, et al. Temperature and precipitation associate with ischemic stroke outcomes in the United States. J Am Heart Assoc. 2018;7(22):e010020.
doi pubmed pmc - Fujii T, Arima H, Takashima N, Kita Y, Miyamatsu N, Tanaka-Mizuno S, Shitara S, et al. Seasonal variation in incidence of stroke in a general population of 1.4 million Japanese: the Shiga stroke registry. Cerebrovasc Dis. 2022;51(1):75-81.
doi pubmed - Wang X, Cao Y, Hong D, Zheng D, Richtering S, Sandset EC, Leong TH, et al. Ambient temperature and stroke occurrence: a systematic review and meta-analysis. Int J Environ Res Public Health. 2016;13(7):698.
doi pubmed pmc - Rothwell PM, Wroe SJ, Slattery J, Warlow CP. Is stroke incidence related to season or temperature? The Oxfordshire Community Stroke Project. Lancet. 1996;347(9006):934-936.
doi pubmed - Khan FA, Engstrom G, Jerntorp I, Pessah-Rasmussen H, Janzon L. Seasonal patterns of incidence and case fatality of stroke in Malmo, Sweden: the STROMA study. Neuroepidemiology. 2005;24(1-2):26-31.
doi pubmed - Ogata T, Kimura K, Minematsu K, Kazui S, Yamaguchi T, Japan Multicenter Stroke Investigators C. Variation in ischemic stroke frequency in Japan by season and by other variables. J Neurol Sci. 2004;225(1-2):85-89.
doi pubmed - Takizawa S, Shibata T, Takagi S, Kobayashi S, Japan Standard Stroke Registry Study G. Seasonal variation of stroke incidence in Japan for 35631 stroke patients in the Japanese Standard Stroke Registry, 1998-2007. J Stroke Cerebrovasc Dis. 2013;22(1):36-41.
doi pubmed - Bucke P, Henkes H, Arnold G, Herting B, Juttler E, Klotzsch C, Lindner A, et al. Seasonal patterns and associations in the incidence of acute ischemic stroke requiring mechanical thrombectomy. Eur J Neurol. 2021;28(7):2229-2237.
doi pubmed pmc - Censi F, Calcagnini G, Mattei E, Calo L, Curnis A, D'Onofrio A, Vaccari D, et al. Seasonal trends in atrial fibrillation episodes and physical activity collected daily with a remote monitoring system for cardiac implantable electronic devices. Int J Cardiol. 2017;234:48-52.
doi pubmed - Sun Z, Bello-Roufai M, Wang X. RNAi inhibition of mineralocorticoid receptors prevents the development of cold-induced hypertension. Am J Physiol Heart Circ Physiol. 2008;294(4):H1880-1887.
doi pubmed - Keatinge WR, Coleshaw SR, Cotter F, Mattock M, Murphy M, Chelliah R. Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombosis in winter. Br Med J (Clin Res Ed). 1984;289(6456):1405-1408.
doi pubmed pmc - Kwok CS, Aslam S, Kontopantelis E, Myint PK, Zaman MJ, Buchan I, Loke YK, et al. Influenza, influenza-like symptoms and their association with cardiovascular risks: a systematic review and meta-analysis of observational studies. Int J Clin Pract. 2015;69(9):928-937.
doi pubmed pmc - Kulick ER, Alvord T, Canning M, Elkind MSV, Chang BP, Boehme AK. Risk of stroke and myocardial infarction after influenza-like illness in New York State. BMC Public Health. 2021;21(1):864.
doi pubmed pmc - Shah AS, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, Langrish JP, et al. Short term exposure to air pollution and stroke: systematic review and meta-analysis. BMJ. 2015;350:h1295.
doi pubmed pmc - Niu Z, Liu F, Yu H, Wu S, Xiang H. Association between exposure to ambient air pollution and hospital admission, incidence, and mortality of stroke: an updated systematic review and meta-analysis of more than 23 million participants. Environ Health Prev Med. 2021;26(1):15.
doi pubmed pmc - Ghoreishi A, Arsang-Jang S, Sabaa-Ayoun Z, Yassi N, Sylaja PN, Akbari Y, Divani AA, et al. Stroke care trends during COVID-19 pandemic in Zanjan Province, Iran. From the CASCADE Initiative: statistical analysis plan and preliminary results. J Stroke Cerebrovasc Dis. 2020;29(12):105321.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
