| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://www.neurores.org |
Case Report
Volume 12, Number 3, October 2022, pages 128-131
Conservative Management for an Infratentorial Pial Arteriovenous Fistula in an Elderly Patient: A Case Report
Paula Ebolia, b, c, Daniel Changa, Robin Babadjounia
aDepartment of Neurosurgery, Cedars-Sinai Medical Center, Los Angeles, CA 90048, USA
bDepartment of Neurosurgery, Torrance Memorial Medical Center, Torrance, CA 90505, USA
cCorresponding Author: Paula Eboli, Department of Neurosurgery, Torrance Memorial Medical Center, Torrance, CA 90505, USA
Manuscript submitted March 21, 2022, accepted June 1, 2022, published online June 16, 2022
Short title: Conservatively Management of pAVF in Elderly
doi: https://doi.org/10.14740/jnr726
| Abstract | ▴Top |
Pial arteriovenous fistulas (pAVFs) are rare vascular malformations requiring intervention in neonates and infants, but the natural course in the elderly population remains unclear. We describe the case of a 78-year-old man with transient symptoms of vertigo and diplopia. Workup including magnetic resonance imaging (MRI) and computed tomography angiography (CTA) demonstrated no acute infarct or hemorrhage to explain the symptoms, but a vascular lesion was noted in the right cerebellum. Digital subtraction angiography confirmed the diagnosis of a pAVF. After review of the literature and discussion with the patient, conservative monitoring with serial imaging was elected. The patient was followed up with repeat CTA which demonstrated stable findings, and the patient remained at his neurologic baseline on long-term follow-up. pAVFs are often symptomatic lesions when found in neonates and infants, necessitating intervention. The findings of these lesions in the elderly (> 70 years of age) are exceedingly rare in the literature and may follow a benign natural course. Without direct evidence of associated symptoms or pathologic findings, conservative management with serial imaging may be a reasonable option for incidentally found pAVFs.
Keywords: Pial arteriovenous fistula; Vascular malformations; Endovascular treatment; Surgical treatment
| Introduction | ▴Top |
Intracranial pial arteriovenous fistulas (pAVFs) are rare vascular malformations, so the incidence and prevalence in general population are unknown, but they comprise approximately 1.6-4.7% of all cerebral arteriovenous malformations (AVMs) [1, 2]. pAVF consists of one or more arterial feeders draining directly into a venous channel. This results in high venous blood flow, leading to varix formation and risk of hemorrhage. pAVFs can be found anywhere in the brain parenchyma, but they tend to be most commonly found in the supratentorial than in the infratentorial region. Most pAVFs are congenital in nature and tend to manifest clinically in childhood or early adulthood and less likely later in life, but they can also be acquired [3]. Clinical presentation varies, and patients can be asymptomatic or experience different neurological symptoms, such as seizures, headaches or focal neurological deficit. pAVFs can even be fatal in case of intracranial hemorrhage and for this reason these lesions are treated in the majority of the cases [4]. In general, the preferred treatment is interruption of the feeding vessels, either through endovascular or surgical techniques.
The majority of studies in the literature consist of retrospective reviews and case reports or small case series. While the ominous course and treatment of these lesions are well described in infants and children, there remains a paucity of information to guide management in elderly patients, particularly those over 70 years old [5-7].
To our knowledge, this is the first case report of an elderly patient presenting with a pAVF that was treated conservatively with observation.
| Case Report | ▴Top |
Investigations
A 78-year-old man presented to the emergency department with symptoms of vertigo, nausea, and worsening of chronic horizontal diplopia after performing push-ups at home. He had known long-standing history of horizontal diplopia, which was diagnosed by his ophthalmologist over 30 years ago. For this, he had no imaging done and diplopia was assumed to be due to a partial, pupil sparing third nerve palsy, probably due to microvascular disease that corrected well with prisms. Other than that, no significant past medical history or family history was reported. On admission examination, he had a left pupil-sparing oculomotor palsy, his pupil was reactive, and his left eye was laterally deviated at neutral gaze with impaired adduction and upgaze with associated ptosis. This was worse when compared to his baseline palsy, otherwise did not exhibit any other focal neurologic deficits.
Diagnosis
Computed tomography (CT) of the head revealed no acute hemorrhage or infarct. Given the constellation of symptoms, he was thought to have a stroke and thus was given tenecteplase. Patient’s symptoms were transient and normalized during his admission except for his diplopia which improved over time. Magnetic resonance imaging (MRI) of the brain did not reveal any acute infarct or hemorrhage, but CT angiography (CTA) of the head and neck revealed serpiginous vessels in the right cerebellar hemisphere (Fig. 1). Final diagnosis was obtained via digital subtraction angiography, which demonstrated a small direct cerebellar pAVF, filling mainly from distal superior cerebellar artery branches, draining directly into dilated cortical veins with no obvious AVM nidus or aneurysms (Fig. 2).
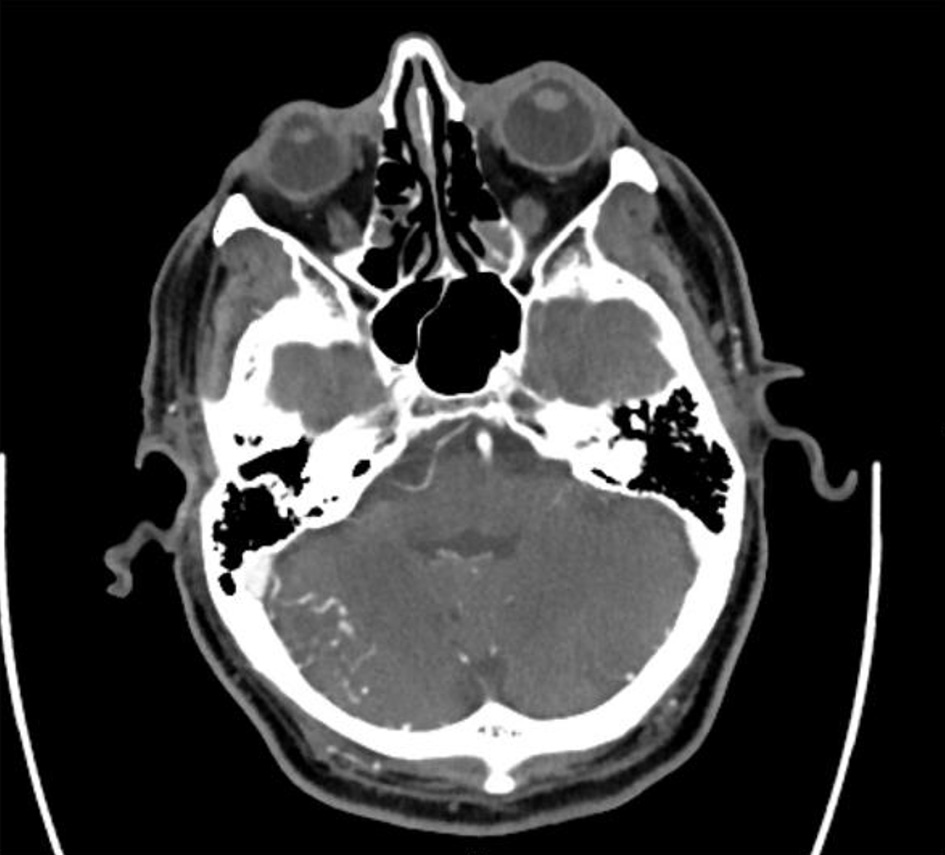 Click for large image | Figure 1. Axial CTA demonstrating serpiginous vessels in the inferolateral aspect of the right cerebellum. CTA: computed tomography angiography. |
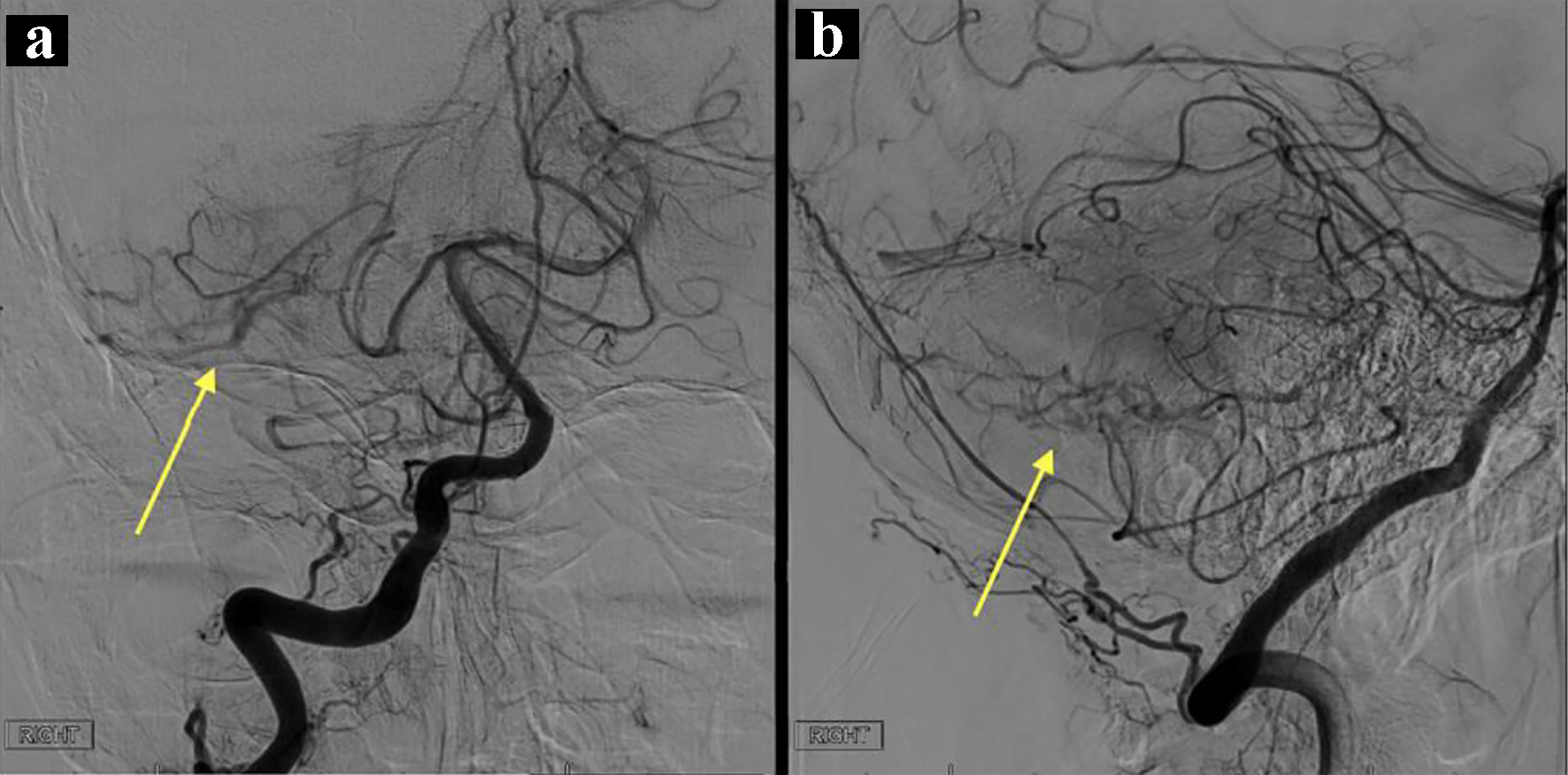 Click for large image | Figure 2. Right vertebral artery angiogram demonstrating a direct pAVF (a and b, yellow arrows) filling from distal superior cerebellar artery branches draining directly into cortical veins without an obvious nidus in the Townes (a) and lateral views (b). pAVF: pial arteriovenous fistula. |
Treatment
Endovascular intervention for embolization was initially offered, but given his advanced age and risks with the procedure, the patient declined and opted instead for observation with serial imaging.
Follow-up and outcomes
The patient was back to his clinical baseline after several days and delayed follow-up CTA demonstrated stable findings (Fig. 3). To date, more than a year from his initial diagnosis, the patient did not experience any hemorrhagic complications and his pAVF has remained stable on multiple follow-up images. He still has his baseline diplopia due to his chronic partial left pupil-sparing oculomotor palsy. On exam, his pupil was reactive, and his left eye was not deviated at neutral gaze with worsening diplopia during adduction, but no ataxia, vertigo or nausea.
 Click for large image | Figure 3. Follow-up axial CTA demonstrating stable serpiginous vessels in the inferolateral aspect of the right cerebellum. CTA: computed tomography angiography; pAVF: pial arteriovenous fistula. |
| Discussion | ▴Top |
Intracranial pAVFs are rare vascular malformations that represent around 1-7% of brain AVM referrals. In pAVF, one or more pial arteries feed directly into a cortical vein without any intervening nidus. It can sometimes be difficult to differentiate them from micro-AVMs which are AVMs whose nidus is smaller than or equal to 1 cm. In general, micro-AVMs are visible on angiography but in some cases only abnormal arterial blood supply or abnormal venous drainage can be found [8]. In these cases, it can be challenging to differentiate micro-AVMs from pAVFs.
pAVFs can be associated with genetic disorders such as Rendu-Osler-Weber syndrome, Ehlers-Danlos, neurofibromatosis type 1, Klippel-Trenaunay-Weber syndrome, but can also be acquired, especially after venous thrombosis, trauma or iatrogenic [5]. They can also be found in association to an already existing AVM or dural AVF [5]. The natural history of pAVFs is not well described secondary to the rarity of these lesions. In the pediatric population, the most commonly found symptoms include heart failure and congestion in neonates, macrocrania or seizures and hemorrhages in infants, and hemorrhages or focal neurologic deficits in adults [9]. It is believed that the high flow shunting of these vessels leads to increased venous pressures and subsequent hydrovenous disorders with symptoms related to shunting effect [10]. This explains the symptoms of heart failure in neonates, demonstrating the most severe form of arteriovenous shunting and early presentation. Patients who survive into adulthood are thought to have compensatory buffering mechanisms to overcome the high flow shunts and can progress to normal living, though remain at risk for hemorrhage [11]. In children, the natural history is very poor with a mortality rate as high as 50%. For this reason, all pAVFs should be treated. On the other hand, adult patients’ natural history is not well understood and may have a more benign course. The symptoms and clinical course can vary widely, with the disease ranging from being asymptomatic to manifesting as transient events, to causing severe neurologic deficits. Adults can most commonly present with seizures, headaches or neurological deficits related to hemorrhages or cerebral ischemic events. It is possible that in the adult population, pAVFs are mainly newly acquired, probably related to a previous trauma or venous thrombosis, and this can somewhat explain its more benign course and different clinical behaviors [3, 12].
The mainstay of treatment for pAVF is disconnection of the arteriovenous shunt either by surgical or endovascular techniques [13]. This differs from AVM management because disconnection alone can eliminate the abnormality avoiding the need for resection. In the case of AVMs, the treatment is based on the resection of the entire lesion making sure no nidus is left behind and that the draining veins are obliterated to avoid collaterals recruitment [14]. While the severity of presenting symptoms in children can be life-saving and warrant immediate intervention, cases like our elderly patient with incidental findings of the pAVF present a dilemma. Even though the theoretical risk of hemorrhage may result in symptoms, surgery itself also entails high risk, particularly in the elderly population. Even while endovascular techniques are considered less invasive, the use of embolic material to address the lesion carries its own risks such as migration of embolic material to draining veins or sinuses, stroke or hemorrhage [15, 16]. Furthermore, the anatomy of the patient such as tortuous vessels or multiple arterial feeders may preclude the possibility of endovascular intervention [17, 18]. Given the inherent risks of intervention combined with the likely compensatory asymptomatic status of elderly patients, it is possible for these patients to ultimately have a benign course. Conservative management with serial imaging may therefore be a considerable option. In these cases, follow-up with serial images is key to rule out potential flow-related feeding aneurysms, progressive enlarging veins and venous outflow obstructions. The literature does not provide a definitive answer for the management of these lesions in elderly patients, but the addition of this case will help add to the repertoire. Further studies evaluating these lesions in this patient population will be needed to help guide practice and best management options.
Conclusion
pAVFs are rare vascular lesions. To our knowledge, this is the only case of an elderly patient (> 70 years of age) presenting with a pAVF that was managed conservatively with observation and long-term follow-up.
In neonates and infants, these lesions often cause significant symptoms, necessitating surgical or endovascular intervention. However, there remains a lack of information to guide the management of pAVFs in the elderly population. Given the present understanding of the mechanisms, conservative management with serial imaging may be a considerable option for patients of this demographic (over 70 years old). Further studies evaluating the long-term outcome and more patient cases will be needed to help bolster our understanding of the natural history of pAVFs.
Acknowledgments
The authors would like to acknowledge and thank the support of their department and institution.
Financial Disclosure
The authors have no financial disclosures concerning the materials or methods used in this study or the findings specified in this paper.
Conflict of Interest
The authors have no conflict of interest to declare.
Informed Consent
The subject of the case report is aware and consented to the case report. The patient’s information was properly anonymized.
Author Contributions
Paula Eboli contributed to drafting and editing of the manuscript, and interpretation of data. Daniel Chang contributed to acquisition of data, and analysis and drafting of the manuscript. Robin Babadjouni contributed to acquisition of data, analysis, and interpretation of data.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Halbach VV, Higashida RT, Hieshima GB, Hardin CW, Dowd CF, Barnwell SL. Transarterial occlusion of solitary intracerebral arteriovenous fistulas. AJNR Am J Neuroradiol. 1989;10(4):747-752.
- Tomlinson FH, Rufenacht DA, Sundt TM, Jr., Nichols DA, Fode NC. Arteriovenous fistulas of the brain and the spinal cord. J Neurosurg. 1993;79(1):16-27.
doi pubmed - Yu J, Shi L, Lv X, Wu Z, Yang H. Intracranial non-galenic pial arteriovenous fistula: A review of the literature. Interv Neuroradiol. 2016;22(5):557-568.
doi pubmed - Nelson PK, Nimi Y, Lasjaunias P, Berenstein A. Endovascular embolization of congenital intracranial pial arteriovenous fistulas. Neuroimaging Clin N Am. 1992;2:309-317.
- Kanai R, Shinoda J, Akatsuka S. Infratentorial pial arteriovenous fistula in the elderly. J Stroke Cerebrovasc Dis. 2015;24(10):e307-309.
doi pubmed - Diana F, Tosatto L, Haznedari N, Commodaro C, Ruggiero M. De novo dural arteriovenous fistula on draining veins of previously treated pial arteriovenous malformation: a case report. J Stroke Cerebrovasc Dis. 2021;30(7):105798.
doi pubmed - Satow T, Suzuki M, Komuro T, Ogawa M, Kobayashi A, Nishida S. Spontaneous resolution of cerebral pial arteriovenous fistula after angiography: report of two cases. World Neurosurg. 2017;103:954.e5-954.e10.
doi
doi pubmed - Hong JF, Song YF, Liu HB, Liu Z, Wang SS. The clinical characteristics and treatment of cerebral microarteriovenous malformation presenting with intracerebral hemorrhage: a series of 13 cases. Biomed Res Int. 2015;2015:257153.
doi pubmed - Hoh BL, Putman CM, Budzik RF, Ogilvy CS. Surgical and endovascular flow disconnection of intracranial pial single-channel arteriovenous fistulae. Neurosurgery. 2001;49(6):1351-1363; discussion 1363-1354.
doi pubmed - Zerah M, Garcia-Monaco R, Rodesch G, Terbrugge K, Tardieu M, de Victor D, Lasjaunias P. Hydrodynamics in vein of Galen malformations. Childs Nerv Syst. 1992;8(3):111-117; discussion 117.
doi pubmed - Duckwiller G. Pediatric Pial AVF. Interv Neuroradiol. 2003;9(Suppl 2):41-46.
doi pubmed - Phatouros CC, Halbach VV, Dowd CF, Lempert TE, Malek AM, Meyers PM, Higashida RT. Acquired pial arteriovenous fistula following cerebral vein thrombosis. Stroke. 1999;30(11):2487-2490.
doi pubmed - Zenteno M, Lee A, Satyarthee GD, Moscote-Salazar LR. Endovascular management of intracranial pial arteriovenous fistulas: experience of largest series at a single center over six years. J Neurosci Rural Pract. 2018;9(3):406-409.
doi pubmed - Meila D, Grieb D, Melber K, Jacobs C, Maslehaty H, Petridis A, El Habony R, et al. Hydrocephalus in vein of Galen malformation: etiologies and therapeutic management implications. Acta Neurochir (Wien). 2016;158(7):1279-1284.
doi pubmed - Giller CA, Batjer HH, Purdy P, Walker B, Mathews D. Interdisciplinary evaluation of cerebral hemodynamics in the treatment of arteriovenous fistulae associated with giant varices. Neurosurgery. 1994;35(4):778-782; discussion 782-774.
doi - Vinuela F, Drake CG, Fox AJ, Pelz DM. Giant intracranial varices secondary to high-flow arteriovenous fistulae. J Neurosurg. 1987;66(2):198-203.
doi pubmed - Smith MD, Russell EJ, Levy R, Crowell RM. Transcatheter obliteration of a cerebellar arteriovenous fistula with platinum coils. AJNR Am J Neuroradiol. 1990;11(6):1199-1202.
- Almeida GM, Shibata MK. Hemispheric arteriovenous fistulae with giant venous dilation. Childs Nerv Syst. 1990;6(4):216-219.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
