| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://www.neurores.org |
Original Article
Volume 11, Number 3-4, August 2021, pages 47-53
Comparison of Code Stroke Response Times Between Emergency Department and Inpatient Settings in a Primary Stroke Center
Catarina De Marchi Assuncaoa, d , Beth Chauncey Eversb, Cassio Henrique Taques Martinsc
, Kerri Remmela
aDepartment of Neurology, University of Louisville, Louisville, KY, USA
bStroke Center, University of Louisville, Louisville, KY, USA
cUniversidade Federal do Parana, Curitiba, Brazil
dCorresponding Author: Catarina De Marchi Assuncao, Department of Neurology, University of Louisville, 401 E Chestnut St Suite 510, Louisville, KY 40202, USA
Manuscript submitted June 4, 2021, accepted July 9, 2021, published online August 19, 2021
Short title: Comparison of Code Stroke Response Times
doi: https://doi.org/10.14740/jnr688
| Abstract | ▴Top |
Background: In stroke, timeliness of care is essential for optimal patient outcomes. While opportunities for code response time improvements have been extensively documented in the medical literature, this retrospective study aimed at providing data and insights for the development of a quality improvement project in the same hospital, with the ultimate goal of increasing code stroke response speeds without compromising the quality of care.
Methods: This was a retrospective cohort study. Data were collected from weekly code stroke review meetings between January and December 2020 from both the emergency department (ED), and inpatient settings from one Joint Commission certified Primary Stroke Center. All code stroke cases with a computed tomography (CT) scan were included. For cases that received tissue plasminogen activator (tPA), variables collected were time from code-to-CT scan start, code-to-tPA, from CT scan start to tPA, and from CT scan completion to tPA. For code stroke cases that did not receive tPA, variables collected were code-to-CT scan start, code-to-CT scan read, from CT scan start to CT scan read, and from CT scan completion to CT scan read. Then, the ED’s code stroke response times were compared with those in the inpatient setting by using a two-tailed t-test and a 95% confidence interval.
Results: From a sample of 206 code stroke activations in 2020, 157 activations met the study’s criteria. For cases that received tPA, the difference in the mean code-to-CT start times between ED and the inpatient settings (9.01 and 24.99 min, respectively) was statistically significant with a P-value < 0.05. For cases that did not receive tPA, the differences between ED and the inpatient settings in the mean code-to-CT start times (14.25 and 30.74 min, respectively) and code-to-CT read times (34.25 and 54.95 min, respectively) were also statistically significant with a P-value < 0.05.
Conclusion: This study highlights the urgent need to improve code-to-CT times in this hospital’s inpatient setting since ED code stroke times were markedly better from a statistical viewpoint. Improving the quality of care will have to address the evident delay in transporting inpatients to the CT scanner after a code stroke has been activated.
Keywords: Stroke; Code; CT; Emergency department; Inpatient; Delays; Response times
| Introduction | ▴Top |
In acute ischemic stroke, timeliness of care is essential for optimal patient outcomes. However, studies have shown that the acute management of a stroke that occurs in an inpatient setting is often delayed compared to management in the emergency department (ED) [1-3]. These delays are usually attributed to code stroke procedures performed by physicians and nurses of the different inpatient services that are lacking in uniformity and standardization [4, 5].
The importance of decreasing code stroke response time stems from the fact that it has been extensively documented in the literature that “time is brain”. By increasing the time efficiency of care, hospitals would automatically improve the quality of care. According to the author of the groundbreaking “Time is Brain - Quantified” study, “every minute in which a large vessel ischemic stroke is untreated, the average patient loses 1.9 million neurons, 13.8 billion synapses, and 7 miles of axonal fibers. Each hour in which treatment fails to occur, the brain loses as many neurons as it does in almost 3.6 years of normal aging” [6]. From the time an inpatient code stroke is activated, unnecessarily delaying stroke care is potentially destroying healthy brain tissue that could have otherwise been better preserved. Thus, stroke hospital teams cannot shy away from seriously tackling this problem.
In light of this issue, the American Stroke Association (ASA), in association with the American Heart Association (AHA), launched in 2010 the Target Stroke Initiative, with the goal to provide door-to-needle (DTN) response times of < 60 min for at least 50% of patients [7]. The intent was that by streamlining emergency stroke care, inpatient stroke response times would also be reduced. By enrolling over 1,200 hospitals across the United States of America, this multidimensional initiative has mainly been successful in improving the timeliness of tPA administration, facilitating the more rapid integration of evidence-based medicine into clinical practice, and, therefore, improving patient outcomes. So much success that in 2014 ASA launched a revised phase II protocol with the ambitious goal of cutting response times to 45 min for at least 50% of patients and below 60 min for at least 75% of patients [8]. In 2019, ASA moved to what it calls phase III, where the goal is to achieve DTN times within 60 min to 85% of patients; DTN within 45 min in 75% or more of acute ischemic stroke patients treated with tPA, and lastly, achieve DTN times within 30 min in 50% or more of acute ischemic stroke patients treated with tPA [9]. Although these initiatives are primarily geared towards emergency stroke response times, hospitals in general use these metrics for quality assessment purposes in inpatient stroke care as well.
Regardless of the standardized ASA guidelines, inpatients will be able to receive tPA in as little time as possible when stroke hospital teams understand how and, most importantly, where lie their most critical delays in code stroke responses so that they can act upon them. Moreover, since there has been customarily more room for stroke response improvements in the inpatient setting due to the lack of attention the topic generally gets, identifying causes for the delays should benefit inpatient care more than the care of patients in the ED setting. Inpatient stroke care has been customarily more cumbersome to improve, but solutions do exist and have the potential to save lives [10].
One of these solutions is highlighted by Garcia-Santibanez et al [4], who also ran a similar study and found that the location of the computed tomography (CT) scanner inside the hospital’s ED was hindering inpatient stroke care. While CT scanners inside the emergency room are a quick and easy way to provide timely stroke care to incoming patients, those already hospitalized need to be transported to a location that is often far from their original room. In this case, it becomes critical that physicians and nurses streamline their inpatient care so much so that the longer time it takes to transport patients to the CT scanner does not become an issue [4].
Inpatients also have the disadvantage of having a higher number of comorbidities in the hospitalized population than the ED’s group, increasing the complexities of hospital practice [11, 12]. Cardiovascular disorders, pulmonary or kidney diseases all predispose to a stroke. In their study, Kimura et al [11] found that in-hospital stroke onset was associated with a history of stroke, being female and the presence of atrial fibrillation (AF). Hospitalized patients tend to be at rest in bed during their hospital stay, which does not bode well for stroke prevention. In AF patients, infection and dehydration are also risk factors for stroke, just like previous stroke or transient ischemic attacks are risk factors for new stroke. Considering this issue, it becomes imperative that nurses and physicians chart out a plan to deal with their patients’ serious comorbidities in advance, so that they know how to act when a code stroke is called [11].
Kassardjian et al [13] demonstrated that the lack of a dedicated algorithm for triaging acute stroke in hospitalized patients is one of the leading causes for inpatient code stroke response delays, as evidenced by Alberts et al as well [14]. Lack of stroke symptom awareness and education, especially among rotating healthcare professionals, continues to hinder proper stroke management [14]. A dedicated protocol or algorithm could help mitigate these issues. For hospital systems that choose not to develop and/or implement new protocols on their own due to budget concerns, there are ways to improve stroke recognition by using adapted in-hospital medical emergency protocols from other hospitals, according to Chen et al [15]. For non-stroke healthcare centers, simply creating a process for rapid referral and transfer to stroke centers may improve outcomes as the most impactful treatment in stroke is a multidisciplinary stroke unit care [15].
Our study aimed to determine whether there was a statistically significant difference between the inpatient and the ED’s code stroke response times in a Joint Commission certified Primary Stroke Center, a major metropolitan hospital in Kentucky. The ultimate goal was for this retrospective study to serve as the theoretical basis for future studies that might propose practical quality improvement interventions in the same hospital.
| Materials and Methods | ▴Top |
Design
A retrospective cohort study of all code strokes that occurred between January 2020 and December 2020 was designed. This study was approved by the ethics committee in compliance with all the applicable University of Louisville ethical guidelines, an institution that adheres to the Declaration of Helsinki Ethical Principles for Medical Research, 1964.
Population
Code stroke events between January and December 2020 were considered. Inclusion criteria were code stroke patients that successfully underwent a CT scan, regardless of intravenous tPA administration or not. Exclusion criteria were the following: any code stroke that after initial evaluation from the neurology service was determined unlikely to be a stroke and did not go to the CT scanner, or any code stroke cases where data were missing. For simplification purposes, code stroke activation was considered T-zero, and as such, door-to-CT (DTCT) and door-to-needle (DTN) times for ED code stroke cases were taken to be analogous to inpatient “code stroke to (start of) CT scan” and “code stroke to tPA administration” respectively.
Data collection
Data were collected from weekly code stroke case reviews. For code stroke cases that underwent thrombolysis, variables collected were time from code stroke (activation) to CT scan (or DTCT for the ED group), time from code stroke (activation) to tPA administration (or DTN for the ED group), time from the start of CT scan to tPA, and time from completion of CT scan to tPA. For code stroke events that did not undergo thrombolysis, variables collected were time from code stroke (activation) to CT scan, time from code stroke (activation) to CT scan read, time from the start of CT scan to CT scan read, and time from completion of CT scan to CT scan read. All cases were divided into two groups depending on where the code stroke was called: ED or inpatient setting. For each variable, the mean and 95% confidence intervals (CIs) were calculated. All variables were measured in minutes. Variables were compared between the two groups using the two-tailed t-test, and a P-value of < 0.05 was considered statistically significant.
| Results | ▴Top |
Between January and December of 2020, there were a total of 206 code stroke activations in our hospital. While 101 of those activations occurred in the ED group, 105 activations occurred in the inpatient setting. Nine cases had to be excluded from the ED group after not meeting the study’s criteria from these numbers. On the inpatient side, 40 patients were excluded for failing one or all of the inclusion criteria. Regarding the other 92 ED code stroke cases that did meet the study’s criteria, 67% had a DTCT response time within 15 min. In the inpatient group, only 12% had a code-to-CT time of < 15 min. In the end, only 10 cases received tPA in the ED group, and one was sent to endovascular intervention. On the inpatient flow, five received tPA, and three others were sent to endovascular intervention. Regarding the 10 cases activated in the ED that received tPA, only three of the 10 received it within 30 min. In the inpatient setting, two of the five cases that received tPA were able to accomplish the task within 30 min (Fig. 1).
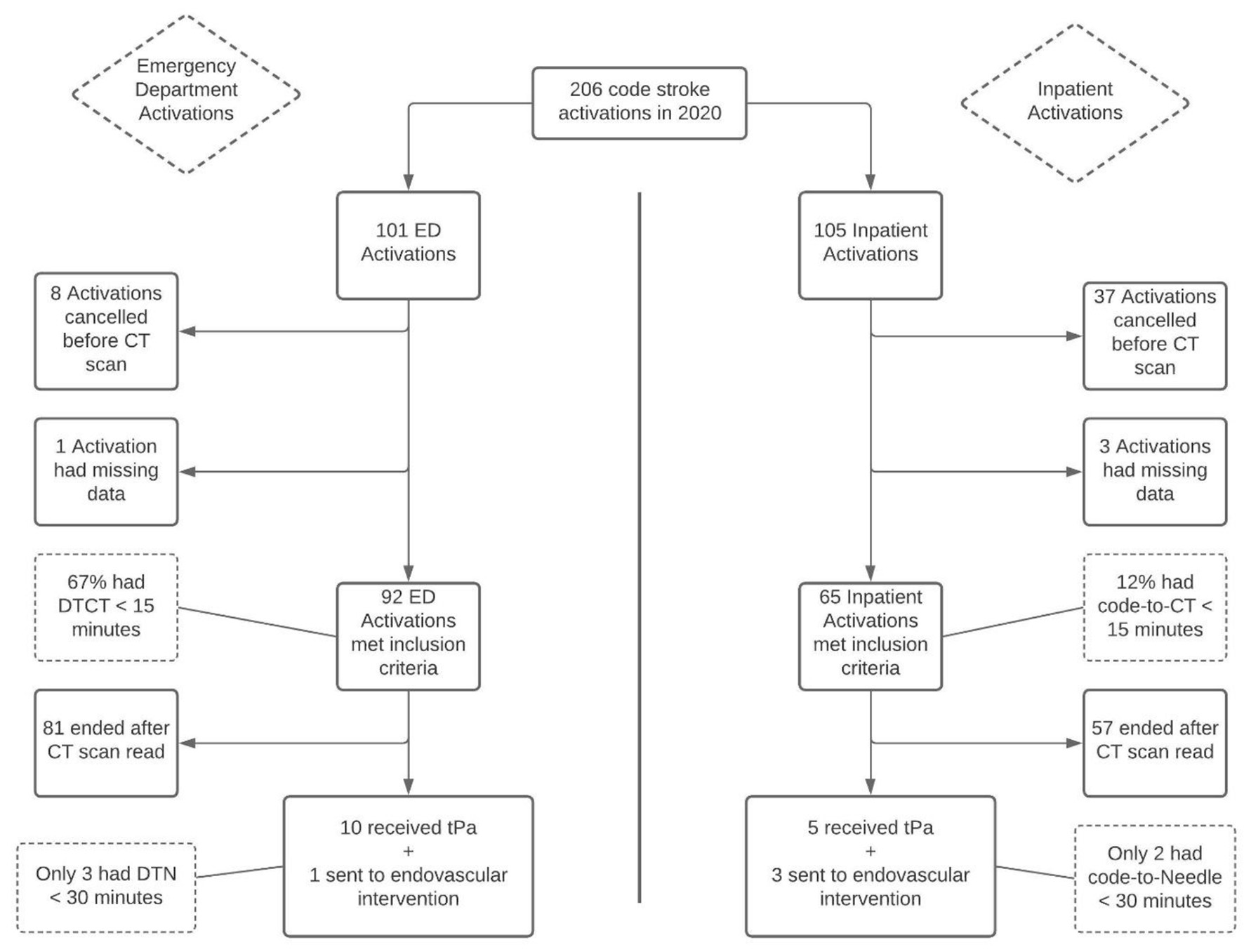 Click for large image | Figure 1. Flowchart of patients included in the study. DTCT: door-to-CT time; DTN: door-to-needle time; CT: computed tomography; tPA: tissue plasminogen activator; ED: emergency department. |
Although they were not part of the exclusion criteria, data from the four patients sent to endovascular interventions (three in the inpatient setting and one in the ED) were also removed from the statistical analysis. In our hospital, requiring the procedure meant transporting patients to another facility. Transportation meant that these four code stroke response times were dramatically higher than the average of the other responses. Including this data would have unfavorably skewed results towards the inpatient setting. Thus, a decision was made to exclude these cases from the statistical calculations.
Regarding the 15 code stroke cases that led to tPA administration, the comparison between ED and inpatient response times is shown in Table 1.
 Click to view | Table 1. Results From Events That Led to tPA Administration |
The mean time it took from code stroke to CT scan (DTCT) in the ED was 9.01 min. In the inpatient group, the same task took on average 24.99 min to be performed, which produces a statistically significant difference with a P-value of < 0.04. The mean time it took from code stroke to tPA administration (DTN) was 61.75 min in the ED and 100.66 min in the inpatient group. Even though the absolute mean numbers are significantly different, this difference had no statistical significance since the P-value was 0.17. Similarly, there was no statistically significant difference between ED and inpatient groups for the time from the start of CT scan to tPA administration (52.75 versus 75.67, P = 0.41). From the completion of CT scan to tPA administration (48.35 versus 61.66 min, P = 0.62), there was also no significant difference even though these absolute mean values clearly show a trend for the inpatient setting to be slower overall.
Regarding the code stroke cases that did meet the study’s inclusion criteria but did not receive thrombolysis or endovascular intervention, a total of 81 patients in the ED group and 57 in the inpatient setting had their times tabulated and compared. Among these 138 code stroke cases, 34 ED and 23 inpatient cases (42% versus 40%, respectively) were from chronic stroke with exacerbation of prior deficits due to ongoing medical problems. Separately, subacute strokes beyond the window of acute interventions also represented a significant portion with 24 ED and 19 inpatient cases (30% versus 34%, respectively). There were also 13 ED and seven inpatient cases (16% versus 12%, respectively) of hemorrhagic strokes that required care outside the code stroke pathway. Tumors represented four ED and five inpatient cases (5% versus 9%, respectively). And lastly, the remaining six ED and three inpatient cases (7% versus 5%, respectively) were attributed to actual ongoing worsening encephalopathy due to medical reasons (delirium) without focal signs, which was later determined to have an onset of more than 24 h.
The comparison between ED and inpatient code stroke response times is tabulated in Table 2.
 Click to view | Table 2. Results From 138 Code Stroke Events That Did not Escalate Beyond a CT Scan |
In this group, the mean time it took from code stroke to start of CT scan (DTCT) in the ED was 14.25 min. In the inpatient group, the same task took on average 30.74 min to be performed, which produces a statistically significant difference with a P-value of 0.0003. The mean time it took from code stroke to CT scan read was 34.25 min in the ED and 54.95 min in the inpatient group, producing a statistically significant difference with a P-value of 0.0213. On the other hand, there were no statistically significant differences between ED and inpatient groups for the time from the start of CT scan to CT scan read (20.00 versus 26.99, P = 0.3099) and for the time from completion of CT scan to CT scan read (14.12 versus 19.76 min, P 0.3808).
| Discussion | ▴Top |
As our results show, there was a statistically significant delay during inpatient code stroke responses, more specifically in the time from code stroke (activation) to CT scan (code-to-CT) when compared to ED response times (DTCT), in both the tPA receiving group and those in the group of patients who did not receive thrombolysis. The difference shows that the inpatient stroke care was not structured and streamlined like the ED setting, especially not in the period between code stroke activation and the CT scan. Response times from code stroke (activation) to tPA administration, on the other hand, had no statistically significant difference. This finding means that once the CT scan was obtained, the time to tPA administration remained the same between ED and inpatients and that the primary source of delays between the two was the time it took to obtain the CT scan. Even so, the absolute mean values for inpatient code stroke response times were higher in all instances.
Identifying the reasons behind delays in obtaining CT scans in the inpatient scenario, when compared to the ED setting, is fundamental to providing streamlined care. Although delayed imaging did not imply an overall delay of tPA administration, it begets room for improvements to be made. Early obtention of imaging is essential not only for tPA or endovascular intervention but also to weed out other types of acute cerebral events and appropriately address them in a timely fashion, such as hemorrhagic strokes and subarachnoid hemorrhages, among many others.
Causes for delayed response in the inpatient setting
This study’s findings align with those found by Garcia-Santibanez et al [4], who also ran a similar study comparing code stroke response times in the ED and inpatient groups in a hospital setting. This statistically significant difference in response times could be explained in many ways, but the first noticeable difference between inpatient and ED settings in our hospital was that the CT scanner was located within the emergency room. While it was easier and quicker for an ED code stroke to obtain scans, an inpatient code stroke required taking patients to a CT scan room often located at a distant location, an architectural disposition also present in many hospitals. However, the actual physical transportation of inpatients to a faraway CT scanner was not the only likely explanation for the discrepancy found in its entirety.
Other possibilities for our hospital’s delayed inpatient code-to-CT times could be because inpatients are much more likely to have comorbidities, increasing the complexities of hospital practice [11, 12]. Previous heart disorders, previous stroke or transient ischemic attacks, and withdrawal of antithrombotic drugs during hospitalization could also predispose inpatients to stroke onset, significantly increasing case complexity and diminishing the odds in favor of a necessary run to the CT scan room within 15 min. It is also suggested by Masjuan et al [1] that apart from delays in contacting the neurologist on stroke call, which could partially explain the delays in some cases, longer response times on the inpatient side could also be due to patients who are more challenging to transport. In this case, patients who are critically ill will get delayed because they are more likely to be connected to intensive care medical equipment, especially if the hospital’s perfusion and respiratory therapy teams are not present and need to be still activated and contacted for disconnection before transport can even be initiated. This scenario was especially true in our hospital, where teams were only activated after Neurology had had a chance to see the patient, delaying transport to the CT scanner even further.
Another possible cause for a delay in our hospital’s inpatient code stroke response could be simultaneous code stroke activations, even though the study’s raw data do not suggest it happened in the period of the study. When Neurology has two or more code strokes active simultaneously, one of those patients will be waiting for longer since transport is not initiated until the Neurology resident or attending has had a chance to look at the stroke candidate. In these rare but unfortunate situations, the nearest available physician should have the authority to order tests and send patients to the CT scanner in order to increase efficiency and prevent further delays, as suggested by Powers et al [9].
Lastly, as highlighted by Kassardjian et al [13], the lack of a dedicated protocol for triaging acute stroke in hospitalized patients is one of the leading causes for inpatient code stroke response delays, as heavily evidenced in other publications as well [14]. The implementation of a formal protocol for managing acute in-hospital stroke could successfully expedite and improve the quality of care.
Another cause for a delayed response in the inpatient setting could be due to differences in stroke etiology between the inpatient and ED settings. Cardioembolic stroke is the subtype of ischemic infarction with the highest in-hospital mortality [16], so a higher percentage of this type in the inpatient group when compared to the ED group could explain the delayed response due to higher case complexity. The short-term prognosis of patients with cardioembolic stroke is also poor when compared to other ischemic stroke subtypes [16]. However, the code stroke response procedures should remain unaltered, regardless of whether the possible stroke is cardioembolic in nature or not. So, although it affects prognosis, the etiology of stroke should not affect the initial code response times.
Causes for delayed response in both ED and inpatient settings
The inpatient setting was not the only group with a delayed response in our hospital. As the data suggest, ED code stroke response times are also not fully optimized in light of the ASA stroke guidelines. There were other causes for delays easily identifiable in both groups. As the study of Kassardjian et al [13] suggests, identifiable causes for code stroke response delays in both ED and inpatient settings might include healthcare professionals’ lack of education about ways to correctly identify stroke candidates, delayed notification and activation of code stroke, and poor communication about the need for urgent medical evaluation. This hospital did employ temporary healthcare workers regularly, so a lack of education on the urgency of responses could be a plausible cause for delayed DTCT or code-to-CT response times. Educational training programs put in place might not have been as effective as planned. This possibility suits this hospital well because ED code stroke response times also showed signs of a need for improvement with a DTCT under 15 min in only 67% of cases when the internal goal was 90%. Thus, the educational aspect could also be playing a role in this case, likely in varying degrees between inpatient and ED settings.
Another possible cause for delay in both instances was the lack of a preprogrammed order set for CT and labs. Since this was not exclusive to one setting over the other, both ED and inpatient code stroke responses could benefit from having a preprogrammed order set since most stroke candidate patients end up requiring the same set of labs and going to the CT scanner as our raw data suggested.
Other possible causes for delay in DTN or code-to-needle times for strong tPA candidates could be the lack of a timely and reliable point of care lab team for coagulation tests. Similarly, notifying the pharmacy to bring tPA only after a CT scan has been read does indicate communication was lacking between different healthcare teams. Yang et al [10] suggest it is essential to have interdisciplinary coordination in rapid stroke response. Not coordinating with the lab and pharmacy teams more efficiently could be delaying DTN and code-to-needle response times in our hospital. After all, this was a hospital looking for ways to improve chances of meeting the phase II goals from the ASA Target Stroke Initiative during 2020. Furthermore, only 30% of the ED tPA receiving patients had a DTN in under 30 min, 40% had a DTN in under 45 min, and 70% of ED patients had a DTN in under 60 min. Thus, our hospital was still at phase I of the ASA Target Stroke Initiative guidelines in 2020.
Limitations of the study
The main limitation of our study is the small sample size. Optimal t-test and P-value calculations are done with a sample size ≥ 30. Our sample of tPA receiving events had only 10 ED code stroke events and five inpatient events to include. Thus, although our findings were in line with other similar studies, as referenced, statistical variables should be recalculated once we obtain more data from the years before 2020. The small sample size could also be why there were no statistically significant differences between ED and inpatient code strokes in the DTN or code-to-needle timeframes, even though the mean values were consistently higher for inpatients. It is likely that with a larger sample size, we would also find a delayed impact on tPA administration when the CT scan was delayed. Although an obvious limitation for a comparison study, small-sized populations of patients receiving tPA are the norm of many community hospitals throughout the United States of America, not the exception. In order to mitigate the limiting effects of this study’s small population, when it comes to external validation, we referenced similar studies conducted in other facilities with larger sample sizes to compare findings.
This study also did not collect data on the number of comorbidities each patient had prior to code stroke, which would have been helpful to the discussion. Thus, it was not possible to make comparisons between the inpatient and ED groups in terms of the mean number of comorbidities these patient groups had prior to having a stroke.
Another limitation was the fact that 2020 was a very atypical year, the first year of the coronavirus disease (COVID) pandemic, and thus, results could be skewed in one way or another. Cognizant of this confounding factor, we tested code stroke response times for the first two pre-pandemic months (January and February) against the remaining months of the year. The authors found no statistically significant difference in any of the code stroke response times between pre and post-pandemic months, internally validating the study. The impact of delays due to the donning of additional personal protective equipment (PPE) can also be considered negligible in code stroke response times.
Conclusions
This study suggests that code stroke response times were primarily being delayed in our hospital due to delays in the code-to-CT response in the inpatient setting. The lack of inpatient transportation to the CT scanner room in a timely fashion should be a topic of concern. This study highlights the urgent need to improve code-to-CT times in this hospital’s inpatient setting. Improving the quality of care will have to address the evident delay in transporting patients to the CT scan after a code stroke has been activated, no matter the cause. Improving this critical transport metric ought to automatically improve DTN (or code-to-needle) times in both ED and inpatient settings, as teams learn the importance of getting to the CT scanner as quickly as possible, especially with those patients who need it the most. The ED code stroke response times might also benefit from incremental adjustments made to the inpatient side of code stroke response.
We believe a cultural change is warranted with the implementation of standardized code stroke response. These would address the most critical metric that stood out during the period studied - the delayed response between code stroke activation to the patient being in the CT scanner. Therefore, the authors of this study call for the adoption of a comprehensive new stroke protocol in our institution to prioritize CT first. The idea is to first think of a list of symptoms that would trigger a code stroke and then take the patient to the CT scanner as quickly as possible while also building closer coordination between teams and educating recurrent and ongoing staff. These measures can improve good routines between the teams and help mitigate delays and improve the care provided to patients presenting with stroke. The creation of a new way to approach this topic at our institution may become a valuable model in improving other services in the region as well, with the potential to save dozens of lives every year while preserving better functioning brains.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Not applicable.
Author Contributions
CA and CM authored the manuscript. BE collected the data and aided in the literature review. KR edited the work and aided in the literature review.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Masjuan J, Simal P, Fuentes B, Egido JA, Diaz-Otero F, Gil-Nunez A, Novillo-Lopez ME, et al. In-hospital stroke treated with intravenous tissue plasminogen activator. Stroke. 2008;39(9):2614-2616.
doi pubmed - Saltman AP, Silver FL, Fang J, Stamplecoski M, Kapral MK. Care and Outcomes of Patients With In-Hospital Stroke. JAMA Neurol. 2015;72(7):749-755.
doi pubmed - Farooq MU, Reeves MJ, Gargano J, Wehner S, Hickenbottom S, Majid A, Paul Coverdell National Acute Stroke Registry Michigan Prototype Investigators. In-hospital stroke in a statewide stroke registry. Cerebrovasc Dis. 2008;25(1-2):12-20.
doi pubmed - Garcia-Santibanez R, Liang J, Walker A, Matos-Diaz I, Kahkeshani K, Boniece I. Comparison of Stroke Codes in the Emergency Room and Inpatient Setting. J Stroke Cerebrovasc Dis. 2015;24(8):1948-1950.
doi pubmed - Cumbler E, Zaemisch R, Graves A, Brega K, Jones W. Improving stroke alert response time: applying quality improvement methodology to the inpatient neurologic emergency. J Hosp Med. 2012;7(2):137-141.
doi pubmed - Saver JL. Time is brain—quantified. Stroke. 2006;37(1):263-266.
doi pubmed - Fonarow GC, Smith EE, Saver JL, Reeves MJ, Hernandez AF, Peterson ED, Sacco RL, et al. Improving door-to-needle times in acute ischemic stroke: the design and rationale for the American Heart Association/American Stroke Association's Target: Stroke initiative. Stroke. 2011;42(10):2983-2989.
doi pubmed - Xian Y, Smith EE, Zhao X, Peterson ED, Olson DM, Hernandez AF, Bhatt DL, et al. Strategies used by hospitals to improve speed of tissue-type plasminogen activator treatment in acute ischemic stroke. Stroke. 2014;45(5):1387-1395.
doi pubmed - Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418.
doi - Yang SJ, Franco T, Wallace N, Williams B, Blackmore C. Effectiveness of an interdisciplinary, nurse driven in-hospital code stroke protocol on in-patient ischemic stroke recognition and management. J Stroke Cerebrovasc Dis. 2019;28(12):104398.
doi pubmed - Kimura K, Minematsu K, Yamaguchi T. Characteristics of in-hospital onset ischemic stroke. Eur Neurol. 2006;55(3):155-159.
doi pubmed - Blacker DJ. In-hospital stroke. Lancet Neurol. 2003;2(12):741-746.
doi - Kassardjian CD, Willems JD, Skrabka K, Nisenbaum R, Barnaby J, Kostyrko P, Selchen D, et al. In-patient code stroke: a quality improvement strategy to overcome knowledge-to-action gaps in response time. Stroke. 2017;48(8):2176-2183.
doi pubmed - Alberts MJ, Perry A, Dawson DV, Bertels C. Effects of public and professional education on reducing the delay in presentation and referral of stroke patients. Stroke. 1992;23(3):352-356.
doi pubmed - Chen S, Singh RJ, Kamal N, Hill MD. Improving care for acute in-hospital ischemic strokes-A narrative review. Int J Stroke. 2018;13(9):905-912.
doi pubmed - Arboix A, Alio J. Acute cardioembolic stroke: an update. Expert Rev Cardiovasc Ther. 2011;9(3):367-379.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
