| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Original Article
Volume 10, Number 1, February 2020, pages 3-6
The Trend of In-Hospital Epilepsy and Its Mortality in the USA: A National Analysis During 1997 - 2014
Jared Alexander Stowersa, Neda Ahmadib, Ali Seific, d
aSchool of Medicine, University of Texas Health Science Center at San Antonio, TX, USA
bUniversity of Texas at San Antonio, TX, USA
cDepartment of Neurosurgery and Neurology, University of Texas Health Science Center at San Antonio, TX, USA
dCorresponding Author: Ali Seifi, Department of Neurosurgery and Neurology, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Drive, San Antonio, TX 78229, USA
Manuscript submitted December 31, 2019, accepted January 7, 2020
Short title: Trend of Epilepsy in the USA
doi: https://doi.org/10.14740/jnr563
| Abstract | ▴Top |
Background: This study focuses on the trend of prevalence of epilepsy hospital discharges in the USA, and the aim is to find any change in the trend of prevalence of epilepsy in the USA and its in-hospital mortality.
Methods: A retrospective cohort study used the Healthcare Cost and Utilization Project (HCUP) national database to analyze trends of epilepsy outcomes between 1997 and 2014.
Results: A total of 4,594,213 total epilepsy discharges were documented between 1997 and 2014 in the HCUP database. The prevalence of annual discharges increased significantly during the study period from 209,002 discharges in 1997 to 280,255 in 2014 (P < 0.0001). There were a total of 35,643 in-hospital deaths due to epilepsy within the cohort during the study period. Mortality of epilepsy decreased across the entire cohort and between genders. In 1997, there were 2,256 documented in-hospital deaths, while 1,759 were recorded in 2014 (P = 0.00157).
Conclusions: Our data showed that the prevalence of hospital epilepsy discharges is increasing in recent years; however, the in-hospital mortality is decreasing. The increase in the prevalence could be due to better detection or increased population, while the improved mortality could be due to better available treatments in recent years. Focusing on designing more accurate and affordable screening tools, as well as targeting further pharmacology-based treatments are an area of research that requires further investigation.
Keywords: Prevalence of epilepsy; Mortality; Health and Cost Utilization Project
| Introduction | ▴Top |
Epilepsy is a neurological disease defined by a subset of diagnostic criteria, of which a patient must meet at least one to receive the medical diagnosis. The conditions for diagnosis of epilepsy include: having at least two unprovoked seizures occurring greater than 24 h apart, one unprovoked seizure and a probability of further seizures similar to the general recurrence risk after two unprovoked seizures occurring over the next 10 years or having a diagnosis of a known epilepsy syndrome [1]. Early definitions of epilepsy focused on unprovoked electrical activity in the brain resulting in unpredictable seizure activity as the basis for definition. However, due to the ambiguous nature of former definitions of epilepsy, the International League Against Epilepsy (ILAE) designated a task force to delineate a more comprehensive definition of the disease, and in 2013 the organization approached the current criteria-based diagnosis [1]. After public comment and discussion, in 2017, the ILAE broadened their definition to include the etiology of the seizure type and, subsequently, the epilepsy type [2]. Knowing the prevalence of epilepsy in our community can bring more information to prepare more strategic plans in controlling its complications and mortality. Our study focuses on the trend of prevalence of epilepsy hospital discharges in the USA, and the aim is to find any change in the trend of prevalence of epilepsy in the USA and its in-hospital mortality.
| Materials and Methods | ▴Top |
We performed a retrospective cohort study using the Healthcare Cost and Utilization Project (HCUP) national database to analyze trends of epilepsy outcomes between 1997 and 2014, specifically focusing on changes in number of annual discharges and inpatient deaths [3]. We identified discharges of patients who were admitted for epilepsy by using the Clinical Classification Software (CCS) code 83 for epilepsy. The definition of the CCS code 83 is described in the Supplementary Material 1 (www.neurores.org). We compiled total values of discharges and in-hospital deaths, and we compared the data against different demographic categories such as gender. Trends during the 18 years of study were evaluated using the z-test statistic and P values using a two-tail test with a significance of less than 0.05. The University of Texas Health at San Antonio exempted this analysis from full review by the Institutional Review Board.
| Results | ▴Top |
Demographics
A total of 4,594,213 total epilepsy discharges were documented between 1997 and 2014 in the HCUP database. The prevalence of annual discharges increased significantly during the study period from 209,002 discharges in 1997 to 280,255 in 2014 (P < 0.0001). All subset demographics that we analyzed within the cohort showed a similar trend, with increases in number of epilepsy discharges from 1997 to 2014. The mean age of the cohort had a very slight variation during the study period, with a mean age of 41.70 years old. In 1997, the mean age of discharged patients was 41.89 years old, and in 2014 it was 41.70 years old (P = 0.86). When scrutinized by gender, females had an older mean age than males. During the study period, the mean female age was 43.72 years old, while males were 39.78 years old. Both males and females saw increases in annual discharges between 1997 and 2014 (P = 0.0000). Male discharges increased from 107,184 in 1997 to 139,810 in 2014 (P = 0.0000), while discharges of females increased from 101,810 to 140,420 (P = 0.0000, Fig. 1).
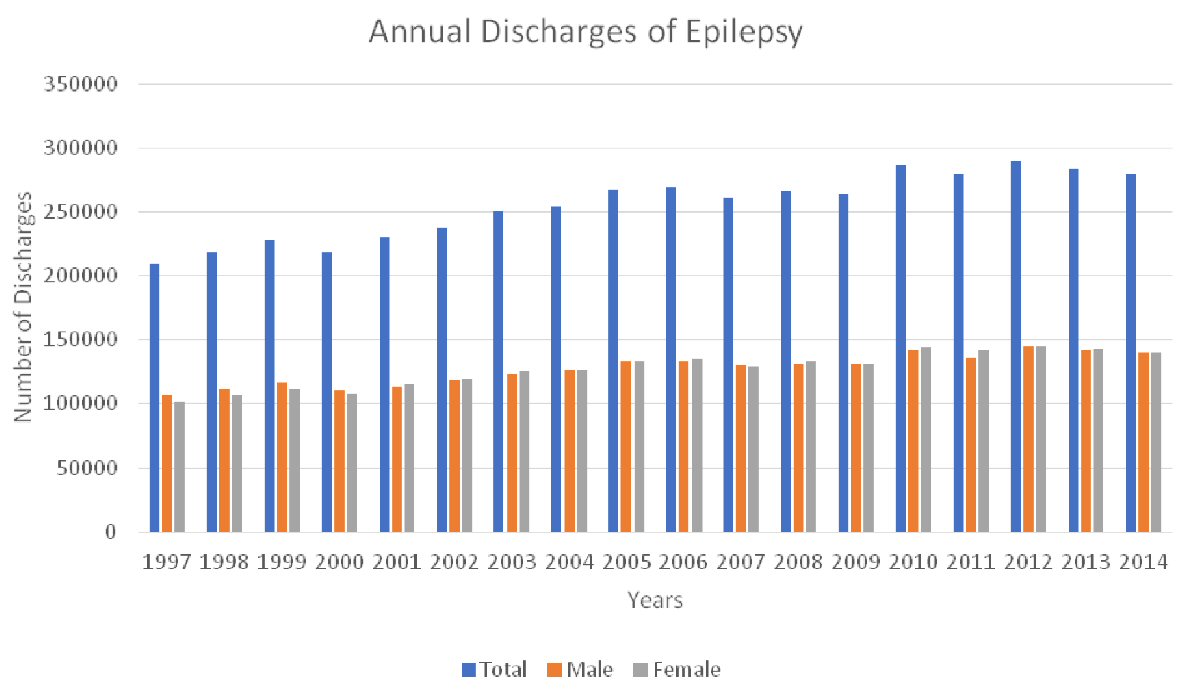 Click for large image | Figure 1. Trend of annual hospital discharges with epilepsy in the USA during 1997 and 2014. |
In-hospital deaths
There were a total of 35,643 in-hospital deaths due to epilepsy within the cohort during the study period. Despite our finding of increased discharges with a principal diagnosis of epilepsy during the study period, we found that the number of in-hospital deaths associated with a principle diagnosis of epilepsy has decreased across the entire cohort and between genders. In 1997, there were 2,256 documented in-hospital deaths, while 1,759 were recorded in 2014 (P = 0.00157). Males and females both faced a similar decrease in mortality during the study period. There were 1,091 male deaths documented in 1997, while 819 deaths in males were reported in 2014 (P = 0.00793). Females recorded 1,164 deaths in 1997 and 939 deaths in 2014 (P = 0.0394, Fig. 2).
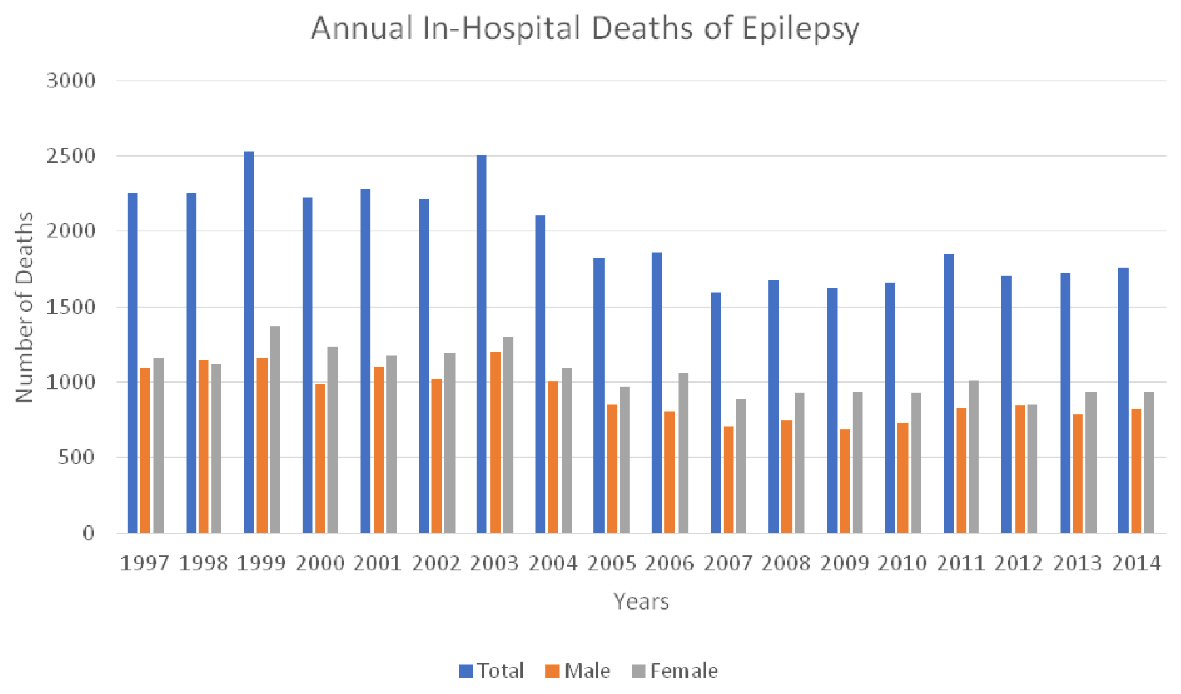 Click for large image | Figure 2. Trend of annual in-hospital deaths for the epilepsy in the USA during 1997 - 2014. |
| Discussion | ▴Top |
Our study determined that there has been an increase in the prevalence of epilepsy, yet a decrease in the hospital mortality during almost two decades in the USA. The average age of discharge of patients discharged with a primary diagnosis of epilepsy remained consistent over the study period at 41.7 years. This increase in the prevalence is aligned with the recent CDC (Centers for Disease Control and Prevention) press release report in 2017. Based on the CDC report, the number of adults with active epilepsy rose from 2.3 million in 2010 to 3 million in 2015. The number or children with the condition increased from 450,000 in 2007 to 470,000 in 2015. These increases are likely due to population growth [4].
One factor that can explain potentially the increase in prevalence of epilepsy is better detection modalities in conjunction with improved diagnostic tools such as continuous electroencephalogram (EEG) monitoring in recent years. For example, Maziero et al discussed in a 2017 paper the promise that exists in continued research in electroencephalography-correlated functional magnetic resonance imaging (EEG-fMRI), which is an evaluation tool that uses multiple diagnostic modalities to develop precise mapping of the brain in patients with focal seizure activity [5]. Increased wide-spread access to EEG monitoring in medical centers in conjunction with enhanced diagnostic modalities and continuing research has likely resulted in better detection of the disease itself. Population growth is another factor that has likely contributed to the rise in annual discharges, as the prevalence of epilepsy within the USA is expected to increase with the rise in population.
Our analysis showed a significant decrease in the hospital mortality of epilepsy. Mortality due to epilepsy is a significant concern. Patients with epilepsy have a mortality rate significantly higher than that of the general population. The standardized mortality rate (SMR) is shown to be 1.6 - 9.3 times higher in this population [6].
Our finding of decreased mortality differed from the study of Greenlund et al [7]. They found that overall, age-adjusted mortality rates per 100,000 population for epilepsy as any-listed cause of death significantly increased from 0.58 in 2005 to 0.85 in 2014 [7]. One possible reason for this discrepancy is that we considered the in-hospital epilepsy death and the Greenlund group considered all epilepsy deaths per 100,000 population. Also, they did not consider status epilepticus in their inclusion criteria which could also be another potential reason for the difference in findings.
In addition to superior detection modalities, improvements in epilepsy treatment and management during the study period have likely contributed to the down-trending in mortality despite the increase in prevalence of epilepsy. A review published in the Journal of Neurology suggests that a better utilization of anti-epileptic drugs in conjunction with a broadened view of individual patient characteristics has helped make epilepsy treatment more effective [8]. Currently, there is substantial ongoing research to further improve epilepsy therapy. Symonds et al discusses the potential prospects in genetic analysis in targeted epilepsy treatment. Symonds discusses the implementation of genetic sequencing allowing for identification of genes pertinent to epilepsy pathogenesis. Certain genetic markers such as the gamma-aminobutyric acid (GABA) and N-methyl-D-aspartate (NMDA) receptors are of particular importance, as they have been associated with both focal seizure activity as well as development of global epileptic disorders [9]. In addition, Gavvala et al asserts that the frequency of continuous EEG monitoring, particularly in adults who are critically ill requiring intensive care unit treatment, has increased in recent years [10]. Clinicians are increasingly using EEG to detect seizure activity in patients with traumatic brain injury, ischemic neurovascular events and comatose states whereas they may not have used monitoring modalities with the same frequency or duration in the past.
Conclusions
Our data showed that the prevalence of hospital epilepsy discharges is increasing in recent years; however, the in-hospital mortality is decreasing. The increase in the prevalence could be due to better detection or increased population, while the improved mortality could be due to better available treatments in recent years. Focusing on designing more accurate and affordable screening tools, as well as targeting further pharmacology-based treatments are an area of research that requires further investigation. As guidelines improve to delineate more focused protocol for EEG implementation, imaging modalities and pharmacology, it is likely that epilepsy statistics will continue to improve.
| Supplementary Material | ▴Top |
Suppl 1. CCS Code 83 (Epilepsy; Convulsions) Including the Following ICD-9 Codes.
Acknowledgments
None to declare.
Financial Disclosure
Authors have no financial disclosure relevant to this article.
Conflict of Interest
Authors have no conflict of interest relevant to this article.
Informed Consent
Not applicable.
Author Contributions
JAS: writing the manuscript and primary analysis; NA: reviewing and editing the article; AS: mentor and design of the project.
Data Availability
The data supporting the findings of this study are available to public at: https://hcupnet.ahrq.gov/#setup
| References | ▴Top |
- Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, Engel J, Jr., et al. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014;55(4):475-482.
doi pubmed - Scheffer IE, Berkovic S, Capovilla G, Connolly MB, French J, Guilhoto L, Hirsch E, et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):512-521.
doi pubmed - https://www.hcup-us.ahrq.gov/.
- https://www.cdc.gov/media/releases/2017/p0810-epilepsy-prevalence.html
- Maziero D, Velasco TR, Salmon CEG, Morgan VL. Two-dimensional temporal clustering analysis for patients with epilepsy: detecting epilepsy-related information in EEG-fMRI concordant, discordant and spike-less patients. Brain Topogr. 2018;31(2):322-336.
doi pubmed - Shahin N. Sudden Unexpected Death in Epilepsy. 2019. Retrieved December 29, 2019, from https://emedicine.medscape.com/article/1187111-overview.
- Greenlund SF, Croft JB, Kobau R. Epilepsy by the Numbers: Epilepsy deaths by age, race/ethnicity, and gender in the United States significantly increased from 2005 to 2014. Epilepsy Behav. 2017;69:28-30.
doi pubmed - Manford M. Recent advances in epilepsy. J Neurol. 2017;264(8):1811-1824.
doi pubmed - Symonds JD, Zuberi SM, Johnson MR. Advances in epilepsy gene discovery and implications for epilepsy diagnosis and treatment. Curr Opin Neurol. 2017;30(2):193-199.
doi pubmed - Gavvala J, Abend N, LaRoche S, Hahn C, Herman ST, Claassen J, Macken M, et al. Continuous EEG monitoring: a survey of neurophysiologists and neurointensivists. Epilepsia. 2014;55(11):1864-1871.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
