| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Case Report
Volume 3, Number 5, October 2013, pages 163-165
MRI Findings of Oculomotor Nerve Palsy in Mild Traumatic Brain Injury: Case Report and Review of the Literature
Aldo F. Bertia, c, Pedro M. Ramireza, Hoan Phan Tranb
aDepartment of Neurosurgery, University of New Mexico, Albuquerque, NM, USA
bFrontier Neurosurgery, Yakima, WA, USA
cCorresponding author: Aldo F. Berti, MSC10 5615, 1 University of New Mexico, Albuquerque, NM 87131, USA
Manuscript accepted for publication September 25, 2013
Short title: MRI Findings of Oculomotor Nerve Palsy
doi: https://doi.org/10.4021/jnr233w
| Abstract | ▴Top |
Isolated traumatic oculomotor nerve palsy associated with mild traumatic brain injury (TBI) is rarely reported in literature and has not been associated with magnetic resonance imaging (MRI) findings until this case report. We report the case of a 55-year-old man with complete left side traumatic oculomotor nerve palsy, 7 mm non-reactive dilated pupil, and ptosis after a helmeted bicycle accident. Mild sulcal subarachnoid hemorrhage was seen on computed tomography (CT) at presentation. MRI during hospitalization showed contrast enhancement of the cisternal segment of the left oculomotor nerve, near the rootlets as it exits the brainstem. He was followed for 18 months with near resolution of oculomotor nerve palsy, but persisting enhancing lesion on MRI at the third nerve outlet from the brainstem, suggestive of partial avulsion. Isolated oculomotor nerve palsy after mild TBI is extremely rare. After review of the literature, we are the first to show radiographic evidence of injury to the oculomotor nerve in a patient with mild TBI. MRI studies may be helpful in a patient with isolated oculomotor nerve palsy to identify the type of injury to the nerve, to rule out underlying pathology concurrent with the TBI, and may also indicate prognosis for recovery.
Keywords: Traumatic oculomotor nerve palsy; Mild traumatic brain injury; MRI
| Introduction | ▴Top |
Traumatic oculomotor nerve palsy may occur due to direct or indirect trauma to the oculomotor nerve [1, 2]. Radiographic findings such as hematomas and skull base fractures on computed tomography (CT) have been implicated in severe direct injury to the oculomotor nerve [3]. However, oculomotor nerve palsy is rarely associated with mild traumatic brain injury (TBI), Glasgow coma scale (GCS) 14-15, and the literature has no radiographic imaging of the oculomotor nerve in this setting. We report the first case of a patient who suffered oculomotor nerve palsy after mild TBI with correlating magnetic resonance imaging (MRI) contrast enhancement of the oculomotor nerve rootlets.
| Case Report | ▴Top |
This is the case of a 55-year-old right-handed Caucasian male who sustained transient loss of consciousness after a helmeted bicycle accident. His GCS on admission to the emergency department was 15. CT scan of the head showed mild left side traumatic subarachnoid hemorrhage near the vertex. On initial neurosurgical evaluation, the patient had a left side non-reactive pupil dilated at 7 mm, complete ptosis, and lateral deviation of the eyeball with no other focal neurological deficits. Other injuries included multiple rib fractures, left side pneumothorax, and back pain. Ophthalmology evaluation confirmed no evidence of extra ocular pathology to the left globe and recommended use of an eye patch for diplopia. MRI of the brain and stem with gadolinium showed contrast enhancement of the cisternal segment of the oculomotor nerve anterior to the left cerebral peduncle between the posterior cerebral artery and the superior cerebellar artery (Fig. 1A), suggesting partial avulsion injury. The patient had an uneventful 11-day hospitalization and was discharged home with follow-up with neurosurgery and ophthalmology.
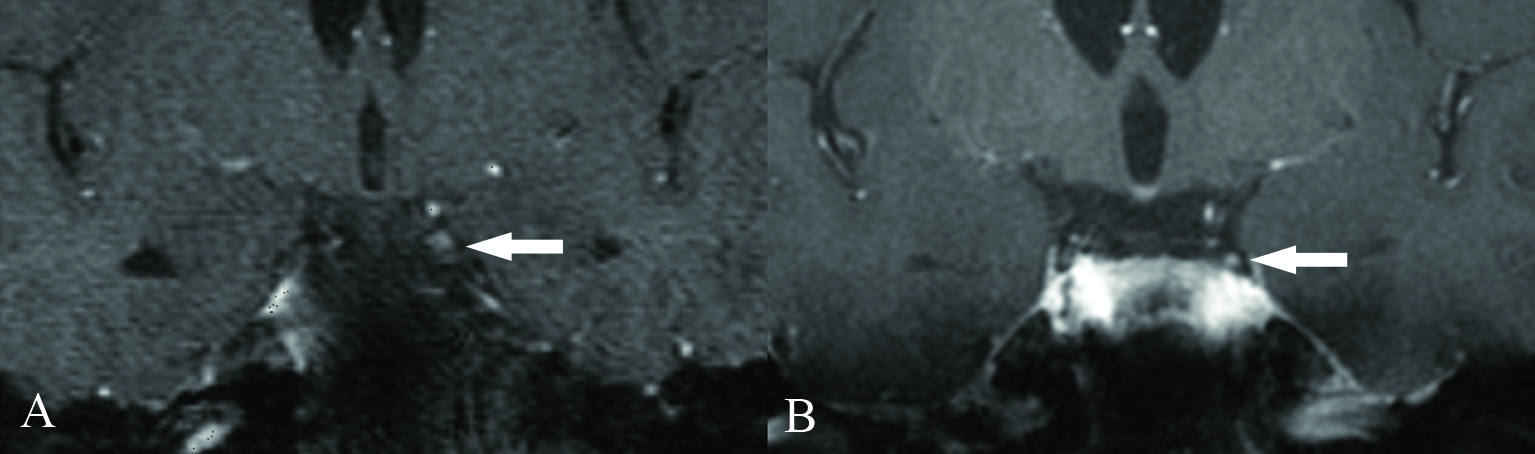 Click for large image | Figure 1. (A) Initial MRI showing contrast enhancement of the left oculomotor nerve rootlets. (B) Follow-up MRI at 18 months shows less but persistent enhancement of left oculomotor nerve, likely representing partial avulsion injury. |
At 6 months follow-up, the patient could open 90% of his eye and maintained a sluggish reactive left pupil. Extraocular motor function was slow in upward and medial movements eliciting diplopia compensated by head tilting. At 18 months follow-up, the patient had complete resolution of ptosis, a sluggish reactive pupil, and slow medial movement of the eye, complaining only of occasional diplopia on right sided gaze. MRI with gadolinium showed less, but persistent, enhancement of the left oculomotor nerve in the cisternal segment in the medial portion of the cerebral peduncle of the midbrain (Fig. 1B).
| Discussion | ▴Top |
Traumatic cranial nerve injuries and sequelae have been extensively reported in association with moderate and severe traumatic brain injuries [1, 4-6]. The cranial nerves most commonly affected were olfactory, facial, and oculomotor in that order [4]. Coello et al reported 49 cases with cranial nerve injuries out of 19,800 (0.25%) patients with mild TBI, of which only 7 (0.04%) had traumatic oculomotor nerve palsy [3]. There are only a few case reports of oculomotor nerve palsy associated with mild TBI in the literature, all of which report no radiographic findings [7-10]. This is the only case report that demonstrates radiographic findings with oculomotor nerve palsy following mild TBI.
Injury to the cranial nerves occurs by indirect and direct mechanisms. Indirect injury occurs from compression, displacement, or deformity of the oculomotor nerve by space occupying lesions [1, 5, 11, 12]. Solomons et al reported oculomotor nerve palsy in 25 out of 2,100 patients; however, most injuries were due to indirect injury of the oculomotor nerve and every patient who suffered traumatic oculomotor nerve palsy had moderate to severe head injury [6]. Muthu et al reported that when isolated oculomotor nerve palsy occurs, the closed head injury must be severe; minor head trauma may precipitate oculomotor nerve palsy in patients with an occult intracranial mass lesion because of the mechanical stress [2]. In such rare cases, the oculomotor nerve may already be stretched or immobilized by an approximating mass rendering it more vulnerable to injury from trauma vectors [11-15].
Direct injuries arise from distraction or contusion of the nerve, rootlet avulsion, distal fascicular damage, or defective blood supply [2, 7, 16]. The most described mechanism of injury is downward displacement of the nerve. The posterior petroclinoid ligament acts as a fulcrum on which the ventromedial pupillomotor fibers of the oculomotor nerve are stretched, sheared, or contused during downward displacement of the brainstem [2, 7, 8, 13, 17]. This propensity to injury is bolstered due to the short distance that the oculomotor nerve has to travel from the midbrain to the supraorbital fissure [2].
Mariak et al reported in a post mortem examination that an isolated group of fibers at the medial aspect of the oculomotor nerve were torn out of the midbrain, suggesting a partial avulsion injury in a patient with severe TBI and primary ophthalmoplegia [18]. Blake et al showed the presence of a residual stump between the superior cerebellar artery and the posterior cerebral artery on coronal MRI indicating complete third nerve avulsion from the brainstem in a severe TBI patient with traumatic nerve palsy; the patient did not recover function [13]. MRI of the brain and stem with gadolinium was performed in our case to rule out an underlying clival or parasellar mass or intracranial aneurysm precipitating the oculomotor palsy. Instead, we identified a contrast enhancing lesion of the cisternal segment of the oculomotor nerve on coronal MRI that could represent a partial avulsion injury on imaging.
Prognosis of isolated traumatic third nerve palsy in mild TBI varies in the literature. Multiple case reports note recovery of intrinsic eye movements and varying degrees of recovery of ptosis and light reflex [7-10]. Coello et al correlated return of function with CT abnormalities and/or skull fractures: 4/7 patients with oculomotor nerve palsy and CT abnormalities (SAH, contusion, or hematoma) recovered full function, whereas 3/7 patients with additional skull base fractures did not recover at 1-year follow-up [3]. Our patient, with evidence of mild sulcal SAH on CT and enhancement of the oculomotor nerve on MRI, had recovered to near normal function on clinical exam, suggesting only a partial avulsion injury clinically.
Conclusion
Oculomotor nerve palsy is rarely associated with mild head injury. A thorough clinical and radiographic evaluation is paramount to identify the injured nerve and rule out concomitant pathology. Because of the paucity of MRI findings of cranial neuropathies in TBI, it is unknown whether enhancement of the oculomotor nerve indicates contusion, avulsion, stretch injury, and so on. Prognosis varies widely in the literature. Further studies are needed, but initial radiographic findings, like this case report, may provide information on the type of injury and give indication for recovery.
Acknowledgments
We thank Dr. Blaine L. Hart, Neuroradiologist at the University of New Mexico Hospital, for his involvement in film interpretation.
Disclosure of Funding
No funding was received for this manuscript.
Financial Support and Industry Affiliations
None of the authors involved have affiliations to any industry or personal or institutional financial interest in any drugs, materials, or devices described in the manuscript.
| References | ▴Top |
- Elston JS. Traumatic third nerve palsy. Br J Ophthalmol. 1984;68(8):538-543.
doi pubmed - Muthu P, Pritty P. Mild head injury with isolated third nerve palsy. Emerg Med J. 2001;18(4):310-311.
doi - Coello AF, Canals AG, Gonzalez JM, Martin JJ. Cranial nerve injury after minor head trauma. J Neurosurg. 2010;113(3):547-555.
doi pubmed - Brazis PW. Isolated palsies of cranial nerves III, IV, and VI. Semin Neurol. 2009;29(1):14-28.
doi pubmed - Memon MY, Paine KW. Direct injury of the oculomotor nerve in craniocerebral trauma. J Neurosurg. 1971;35(4):461-464.
doi pubmed - Solomons NB, Solomon DJ, de Villiers JC. Direct traumatic third nerve palsy. S Afr Med J. 1980;58(3):109-111.
pubmed - Chen CC, Pai YM, Wang RF, Wang TL, Chong CF. Isolated oculomotor nerve palsy from minor head trauma. Br J Sports Med. 2005;39(8):e34.
doi pubmed - Katsuno M, Kobayashi S, Yokota H, Teramoto A. [Primary oculomotor nerve palsy due to mild head injury—report of two cases]. Brain Nerve. 2008;60(1):89-91.
pubmed - Liu YT, Lee YC, Liu HC. Isolated oculomotor nerve palsy due to head injury. J Chin Med Assoc. 2004;67(3):149-151.
pubmed - Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y, Yatsushige H. [Isolated traumatic oculomotor nerve palsy caused by minor head trauma]. Brain Nerve. 2008;60(5):555-558.
pubmed - Eyster EF, Hoyt WF, Wilson CB. Oculomotor palsy from minor head trauma. An initial sign of basal intracranial tumor. JAMA. 1972;220(8):1083-1086.
doi pubmed - Walter KA, Newman NJ, Lessell S. Oculomotor palsy from minor head trauma: initial sign of intracranial aneurysm. Neurology. 1994;44(1):148-150.
doi pubmed - Blake PY, Mark AS, Kattah J, Kolsky M. MR of oculomotor nerve palsy. AJNR Am J Neuroradiol. 1995;16(8):1665-1672.
pubmed - Lesser RL, Geehr RB, Higgins DD, Greenberg AD. Ocular motor paralysis and arachnoid cyst. Arch Ophthalmol. 1980;98(11):1993-1995.
doi pubmed - Park-Matsumoto YC, Tazawa T. Internal carotid-posterior communicating artery aneurysm manifesting as an unusual ocular motor paresis after minor head trauma—case report. Neurol Med Chir (Tokyo). 1997;37(2):181-183.
doi - Heinze J. Cranial nerve avulsion and other neural injuries in road accidents. Med J Aust. 1969;2(25):1246-1249.
pubmed - Skrzat J, Walocha J, Jaworek JK, Mroz I. The clinical significance of the petroclinoid ligament. Folia Morphol (Warsz). 2007;66(1):39-43.
- Mariak Z, Lewko J, Zimnoch L. Pathogenesis of primary internal ophthalmoplegia after head injury. Eur J Ophthalmol. 1995;5(1):56-58.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
