| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Case Report
Volume 2, Number 5, October 2012, pages 221-223
“Severe Neurological Deficit” a Rare Complication Following Spinal Anesthesia
Dheeraj Raia, b, Maneesh Kumar Singha, Ravindra Kumar Garga, Pravin Umakant Naphadea, Tushar Premraj Rauta
aDepartment of Neurology CSM Medical University, Lucknow, India
bCorresponding author: Dheeraj Rai, Senior Resident, Department of Neurology CSMMU, Lucknow, India
Manuscript accepted for publication October 1, 2012
Short title: Severe Neurological Deficit
doi: https://doi.org/10.4021/jnr140w
| Abstract | ▴Top |
Severe neurological deficit following spinal anesthesia is an uncommon incident. Here we report a 24-year-old female who was given spinal anesthesia for lower segment caesarean section developed transient severe pain at the site of needle insertion radiating to right lower limb during the procedure followed by weakness predominantly involving the right lower limb and areflexia. Her magnetic resonance imaging of spine revealed signal intensity alteration in the spinal cord from 5th thoracic segment to the conus suggestive of extensive myelitis along with involvement of nerve roots following the procedure.
Keywords: Spinal anesthesia; Spinal cord injury; Myeloradiculitis; Caesarean section
| Introduction | ▴Top |
Spinal anesthesia is the commonest form of anesthesia used in obstetric practice and ending up in a dreaded complication like spinal cord injury and severe neurological deficit is devastating for the obstetrician, the anesthetist and most of all, the pregnant woman who was only meant to undergo a simple procedure. However it is fortunate that this is an extremely rare complication in today’s medical scenario. Literature says there are few other causes for spinal anesthesia related neurological deficit other than direct needle injury to the spinal cord or nerves which includes spinal cord ischemia, neurotoxicity due to drugs administered, spinal hematoma formation and infection [1, 2]. Here we report a case of severe neurological deficit due to direct spinal cord injury during spinal anesthesia and subsequent involvement of nerve roots.
| Case Report | ▴Top |
A 24-year-old woman, para 2 living 2 who underwent elective lower segment caesarian section (LSCS) at a peripheral centre 10 days back was referred to us for complaints of weakness in her right lower limb which she developed immediately after her caesarian section. Spinal anesthesia was given in sitting position. However, details regarding the indication for the caesarian section, drugs and their dosages used for the spinal anesthesia could not be found out. We elicited a history of transient sharp shooting pain during the insertion of spinal needle which was radiating to her right lower limb. Once the effect of anesthesia wearied off, she noticed an inability to move her right lower limb and numbness over the right side of her body below the costal margin extending over entire right lower limb. However, she did not complain of any sensory loss or weakness in the left half of body and both upper limbs either. For this she was administered intravenous infusion of methylprednisolone 1gram daily from first to fifth post operative day. On the third post operative day, the urinary catheter was removed, when she had two episodes of urinary incontinence due to which the catheter was reinserted on the same day. There were no obstetric complications antenatally, intra and post operatively.
On examination her vital signs were stable, operative wound was healthy and sutures had been removed. Her higher mental functions and cranial nerve examination was normal. Her motor examination revealed hypotonia and foot drop in the affected limb. The power (as assessed by Medical Research Council grading) at right hip, knee and ankle joints were 0/5, 2/5 and 0/5 respectively. Left hip flexors and knee extensors also appeared to be involved with a power of 4/5. Plantar reflex was not elicitable on the right side and was a flexor response on the left. Deep tendon reflexes were absent in both lower limbs except left knee (which was 2+), 50% sensory loss of pain and touch sensation was present in the right lower limb and right half of the body below the level of 6th thoracic spinal level. Joint position and vibration senses were impaired on the right side.
Her routine biochemistry, complete hemogram, renal function, liver functions were normal. Thyroid profile, serum vitamin B12 levels and coagulation studies were also normal. Her cerebrospinal fluid (CSF) analysis showed disproportionate rise in proteins with normal sugars (10 cells, all lymphocytes, proteins 148.2 mg%, sugars 62 mg% and negative for gram and AFB staining). CSF was also sent for anti varicella zoster and anti herpes simplex virus antibodies which came negative.
Magnetic resonance imaging of spine showed signal intensity alteration (T1 isointensity and T2 hyperintensity) in spinal cord extending from 5th thoracic vertebra to terminal part of cord namely conus medullaris with no post contrast enhancement mainly affecting the right half of the cord (Fig. 1).
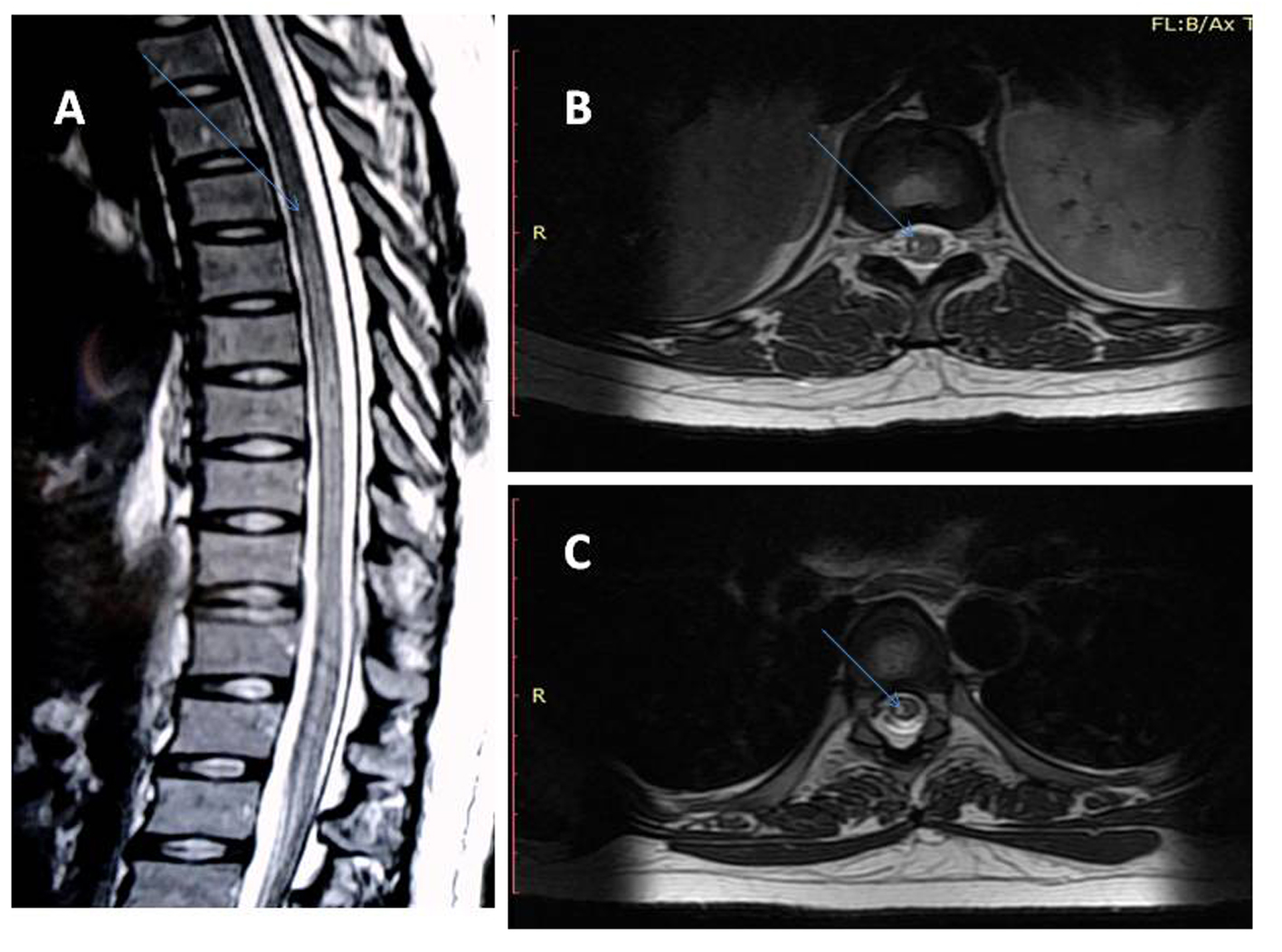 Click for large image | Figure 1. Magnetic resonance imaging of spine T2 weighted image saggital section showing signal intensity alteration (hyperintensity) in the cord extending from T5 to the conus medullaris (A), axial section showing signal alteration in the cord predominantly involving the right half at two different levels (B, C). |
Nerve conduction study of lower limbs showed decrease compound muscle action potentials (CMAPs) in right common peroneal and posterior tibial nerves and normal sural nerve sensory nerve action potential (SNAPs).
Electromyography of Paraspinal and lower limb muscles did not show any spontaneous activity at the time of admission namely 10 days after injury. However repeat study showed spontaneous activity in the form of positive sharp wave and fibrillation potentials after 6 weeks.
As the patient already received methylprednisolone, we only administered supportive treatment and physiotherapy. After 3 months of treatment patient showed signs of improvement in terms of muscle power at hip and knee, which became 4/5 (MRC grading) and that at the ankle became 2/5.
| Discussion | ▴Top |
Obstetric anesthesia has been a double tricky situation for an anesthetist, bearing the fact that two lives have to be safe by the end of the procedure, quite in contrast to other medical situations. Spinal anesthesia has evolved through this as the anesthesia of choice for a cesarean section. Though it has been considered a relatively safe form of anesthesia, it still can have complications like hypotension, post dural puncture headache, backache, total spinal block, cardiovascular collapse and various neurological complications. These neurological complications are fortunately rare amounting to 0.03% [2, 3]. These neurological complications have been classified into three groups (1) Those directly related to anesthesia (2) those unrelated to anesthesia (3) those in which anesthesia is an incidental but possibly a contributory factor [4] There have been various causes of neurological injuries after spinal anesthesia which include direct injury by the needle to the spinal cord or the nerves, spinal cord ischemia, bacterial contamination of the subarachnoid space, drug neurotoxicity and hematoma formation [1, 2]. Kennedy et al [5] were the first ones to note severe neurological deficit following spinal anesthesia described as “grave spinal cord paralysis”. Of a special mention is the infamous incident of Woolley and Roe from England in the year 1947, who suffered major neurological deficits on receiving spinal anesthesia on the same day at the same hospital [6]. After this spinal anesthesia was almost abandoned from clinical practice and only came back in the 1970s. Here we describe an obstetric patient who at the time of needle insertion of spinal anesthesia experienced severe transient sharp shooting pain radiating to right lower limb followed by asymmetric sensory motor paraparesis mainly affecting the right lower limb with areflexia and bladder involvement. MRI of her spine showed signal intensity alteration in the spinal cord extending from T5 level to conus medullaris, mainly in the right half of the cord without contrast enhancement. A probable explanation for this finding would be a possible prick to the spinal cord and subsequent injection of anesthetic drug into it causing inflammation of the cord and its nerve roots (myeloradiculitis). On the contrary to the expectation, contrast enhancement of roots was not found, most likely cause of this being delayed presentation of the case (10 days after the injury). Direct trauma to the spinal cord causing neurological deficits have been described in yet other reports like those of Reynold’s [7] and Netravathi M et al [8]. Intravenous methylprednisolone infusion has been used for treating such cases though with limited benefits. Electrophysiological studies (nerve conduction study and electromyography) should be considered in such patients to rule out peripheral nerve injuries and any pre-existing neurological deficits.
Spinal anesthesia though is a very safe procedure, should be done with meticulous care and caution to avoid such dreaded neurological complications. Appreciation of paraesthesia or sharp radiating pain at time of needle insertion should be taken seriously as it may be the alarm for spinal cord of nerve injury. Needle should be withdrawn immediately and should either be re inserted or an alternative form of anesthesia should be considered to prevent neurological deficits.
| References | ▴Top |
- Fan B, Critchley L. Neurological complications associated with neuraxial block: What are the causes? SAARC J. Anaesth. 2008;1(1):32-38.
- Auroy Y, Benhamou D, Bargues L, Ecoffey C, Falissard B, Mercier FJ, Bouaziz H, et al. Major complications of regional anesthesia in France: The SOS Regional Anesthesia Hotline Service. Anesthesiology. 2002;97(5):1274-1280.
doi pubmed - Moen V, Dahlgren N, Irestedt L. Severe neurological complications after central neuraxial blockades in Sweden 1990-1999. Anesthesiology. 2004;101(4):950-959.
doi pubmed - Bromage PR. Neurological complications of epidural and spinal techniques. Ballieres clin Anesthesiol. 1992; 7: 793-815.
doi - Kennedy F, Effron AS, Perry G. The grave spinal cord paralyses caused by spinal anesthesia. Surg Gynecol Obstet. 1950;91(4):385-398.
pubmed - Cope RW. The Woolley and Roe case; Woolley and Roe versus Ministry of Health and others. Anaesthesia. 1954;9(4):249-270.
doi pubmed - Reynolds F. Damage to the conus medullaris following spinal anaesthesia. Anaesthesia. 2001;56(3):238-247.
doi pubmed - Netravathi M, Taly AB, Sinha S, Bindu PS, Goel G. Accidental spinal cord injury during spinal anesthesia: A report. Ann Indian Acad Neurol. 2010;13(4):297-298.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
