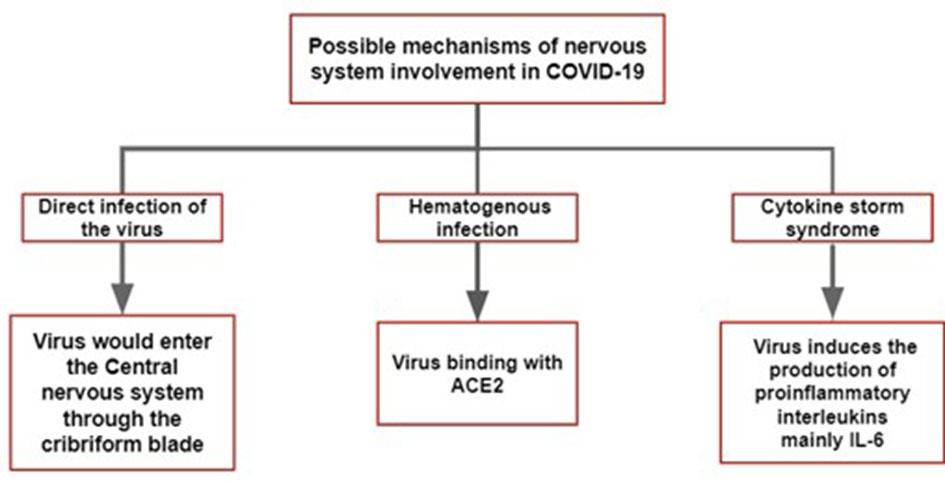
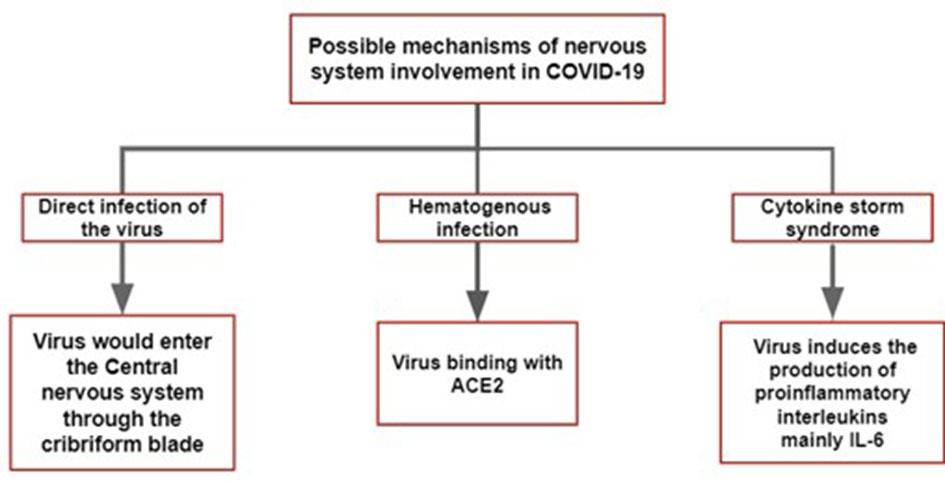
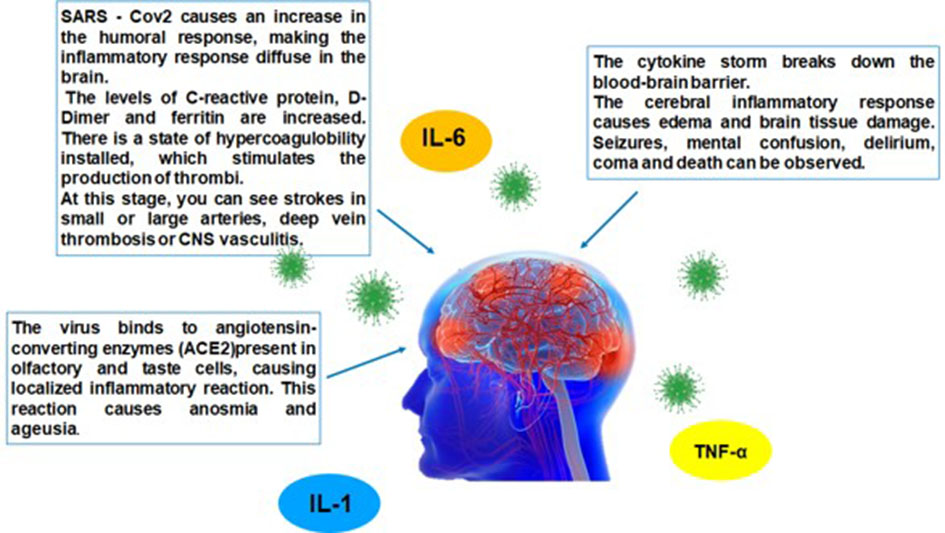
Figure 1. The main hypothesis of the pathophysiological mechanism of COVID-19 in the nervous system. COVID-19: coronavirus disease 2019; ACE: angiotensin-converting enzyme; IL: interleukin.
| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://www.neurores.org |
Review
Volume 10, Number 5, October 2020, pages 164-172
Neurologic Compromise in COVID-19: A Literature Review
Figures
Table
| Reference | Study design | Clinical findings | Comments |
|---|---|---|---|
| COVID-19: coronavirus disease 2019; GBS: Guillain-Barre syndrome; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; PNS: peripheral nervous system; ICU: intensive care unit; RT-PCR: reverse transcription-polymerase chain reaction; CSF: cerebrospinal fluid; CT: computed tomography; PCR: polymerase chain reaction. | |||
| GBS | |||
| Virani et al [9] | Case report of a patient who tested positive for SARS-CoV-2 and developed progressive ascending weakness consistent with GBS. | Numbness and weakness in lower limbs. | Recovery of the symptoms and forwarding to physiotherapy. |
| Caamano and Beato [10] | Case report of a confirmed COVID-19 infection that developed a rare form of GBS. | Facial nerve bilateral paralysis. | Small improvement of the symptoms. |
| Anosmia/ageusia | |||
| Mao et al [4] | A retrospective and observational study which analyzed 214 hospitalized patients with SARS-Cov-2 infection diagnosis laboratory confirmed. | Out of the PNS symptoms, the most reported were impaired taste in 12 patients (5.6%) and impaired smell in 11 patients (5.1%). | - |
| Baig et al [11] | Cross-sectional survey of 1,480 patients with symptoms similar to influenza carried out between March 3 and 29, 2020, evaluated 59 (58%) of 102 COVID-19-positive patients and 203 (15%) of 1,378 COVID-19-negative patients. | Loss of smell and taste was reported in 68% and 71% of subjects positive for COVID-19, respectively, compared to 16% and 17% of subjects in negative patients. | Of the patients who reported the loss of smell associated with COVID-19, 74% (28/38) reported the resolution of anosmia with clinical resolution of the disease. |
| Lechien et al [12] | Multicenter, peer-reviewed study involving 12 European hospitals evaluated 417 patients with COVID-19. | It was observed that 85.6% and 88% had olfactory and gustatory dysfunctions, respectively. | The olfactory dysfunction emerging before other symptoms in 11.8% of cases. The recovery rate was 44% in a short period and women were significantly more greatly affected. |
| Giacomelli et al [13] | Cross-sectional survey collected data from 59 hospitalized patients with SARS-Cov-2 infection with a questionnaire and a formal interview. | This study notices that 11 patients (18.6%) had both taste and olfactory disorders, while 20 patients (33.9%) had at least one of them. | Olfactory dysfunctions were more frequently reported in women and in younger patients. |
| Encephalopathy | |||
| Poyiadji et al [14] | Case report of a woman in her fifties who presented with acute hemorrhagic necrotizing encephalopathy. | The patient presented with cough, fever, and altered mental status. | The authors reported neither patient’s comorbidities nor the outcome of the case. |
| Filatov et al [15] | Case report of a 74-year-old man with acute encephalopathy and altered level of consciousness. | The patient was found encephalopathic, nonverbal, unable to follow any commands, just able to move his extremities and to react to noxious stimuli. | The patient had a past medical history of atrial fibrillation, cardioembolic stroke, Parkinson disease, chronic obstructive pulmonary disease, and recent cellulitis. He developed respiratory failure and was transferred to the ICU. |
| Lu et al [16] | Retrospective multicenter study with 304 patients. | Eight patients were encephalopathic: one as obtunded, one was delirious, and six were comatose. | The most common complication among the patients was hypoxia. |
| Chen et al [17] | Retrospective case series with 274 patients, 113 individuals died and 161 recovered. | Twenty-three deceased patients showed hypoxic encephalopathy. | Symptoms associated with hypoxemia were more common among the patients who died than in those who recovered. |
| Helms et al [18] | Observational study involving 58 patients with acute respiratory distress syndrome due to COVID-19. | Eight patients showed neurological findings on admission to the ICU, and 39 patients showed these symptoms after sedation and administration of a neuromuscular blocker. | All the seven patients who underwent RT-PCR assays of the CSF samples were negative for SARS-CoV-2. |
| Cerebral vascular disease | |||
| Avula et al [19] | Four case reports of patients that presented with imaging confirmed acute stroke and PCR confirmed COVID-19 disease. | Elderly patients, three women and one man. All with previous comorbidities. As they were at the hospital had a CT-detected stroke. | Three patients were deemed not candidates for thrombolysis or neuro-intervention due to poor functional status. Families eventually chose for comfort measures. The oldest patient (88 years old) was discharged to a rehab facility with an event monitor. |
| Saiegh et al [20] | Two case reports of patients with COVID-19 and concurrent neurological symptoms. | A 31-year-old man developed an acute-onset severe headache and loss of consciousness diagnosed with subarachnoid hemorrhage from a ruptured aneurysm. A 62-year-old woman who had an ischemic stroke with hemorrhagic conversion. | Both patients recovered well and were discharged. |
| Gonzalez-Pinto et al [21] | Case report of a 36-year-old woman who was a healthcare worker and smoker. | She was found lying on the floor unable to talk or to move her right side. At the hospital she had a confirmed PCR for COVID-19. | Her level of consciousness gradually deteriorated, and she passed away 72 h after admission. |
| Oxley et al [22] | Five case reports of COVID-19 patients with large vessel stroke under 50 years old. | Four men and one woman had neurological impairment and had confirmed diagnose of stroke on CT. | They had the clot retrieval and received anticoagulant therapy. Three were discharged and two were still at the hospital by the time of the article publication. |
| Other findings | |||
| Tape et al [23] | Case report of a 79-year-old woman. | She arrived at the hospital after a syncopal episode that occurred at her home, experienced fever, and tested positive for COVID-19. | History of coronary artery disease with multiple stents, hypertension, and congestive heart failure. The assessment of the syncope’s etiology revealed orthostatic hypotension. The electrocardiogram did not reveal any arrhythmias. |
| Vollono et al [24] | Case report of a 78-year-old woman with seizures. | She had a previous history of herpetic encephalitis and months later she had focal status epilepticus without any prodromal symptoms. As she got admitted at the hospital, she presented more symptoms and tested positive for COVID-19. | She received antiepileptic treatment and was treated with lopinavir-ritonavir plus hydroxychloroquine. She recovered well. |
| Guan et al [25] | Observational study involving 1,099 Chinese patients. | A total of 164 patients showed myalgia, and 134 of them had non-severe disease. | Sixty-seven patients with non-severe disease and 23 patients with severe disease presented with creatine kinase serum levels ≥ 200 U/L. |