Figures
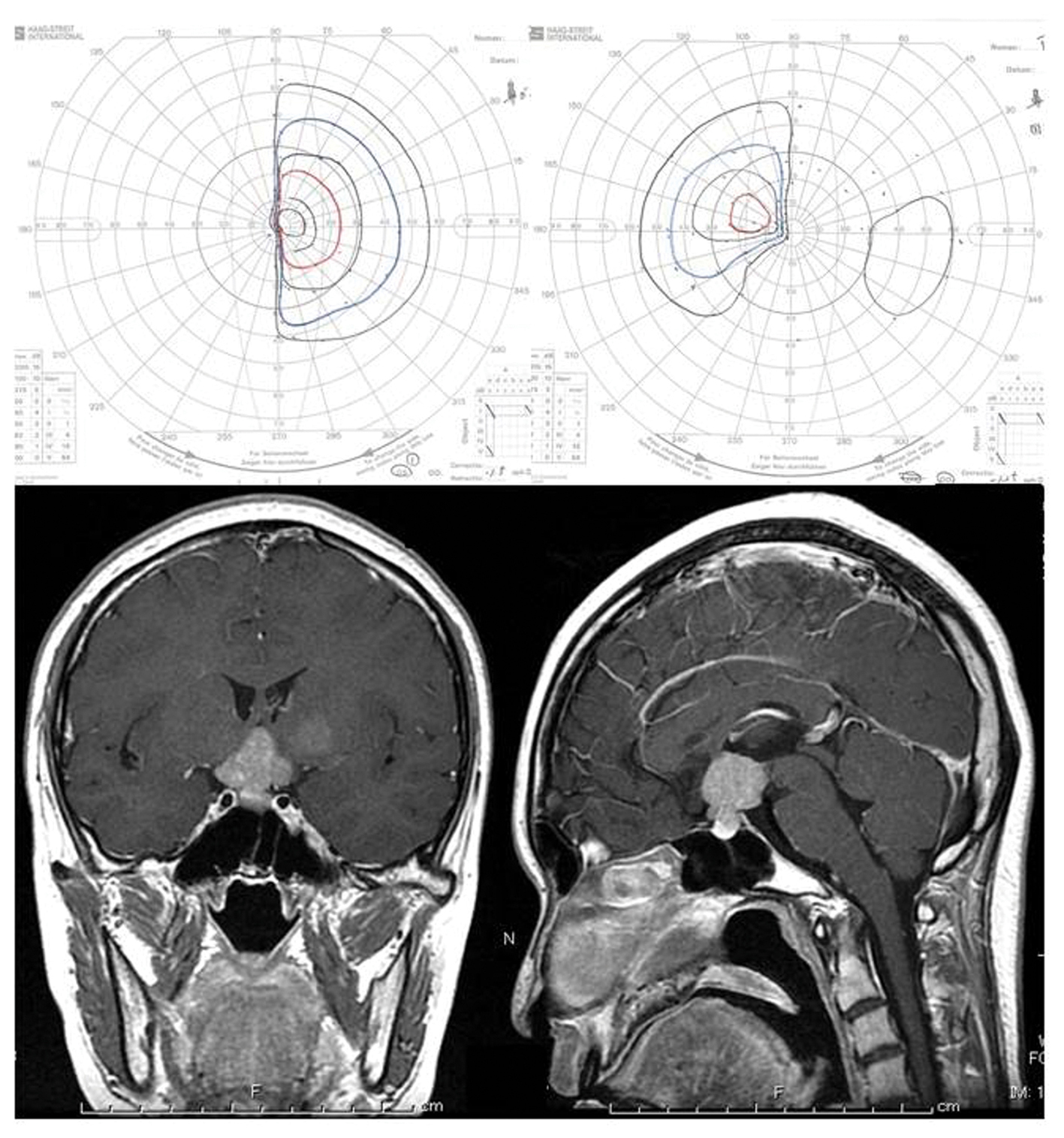
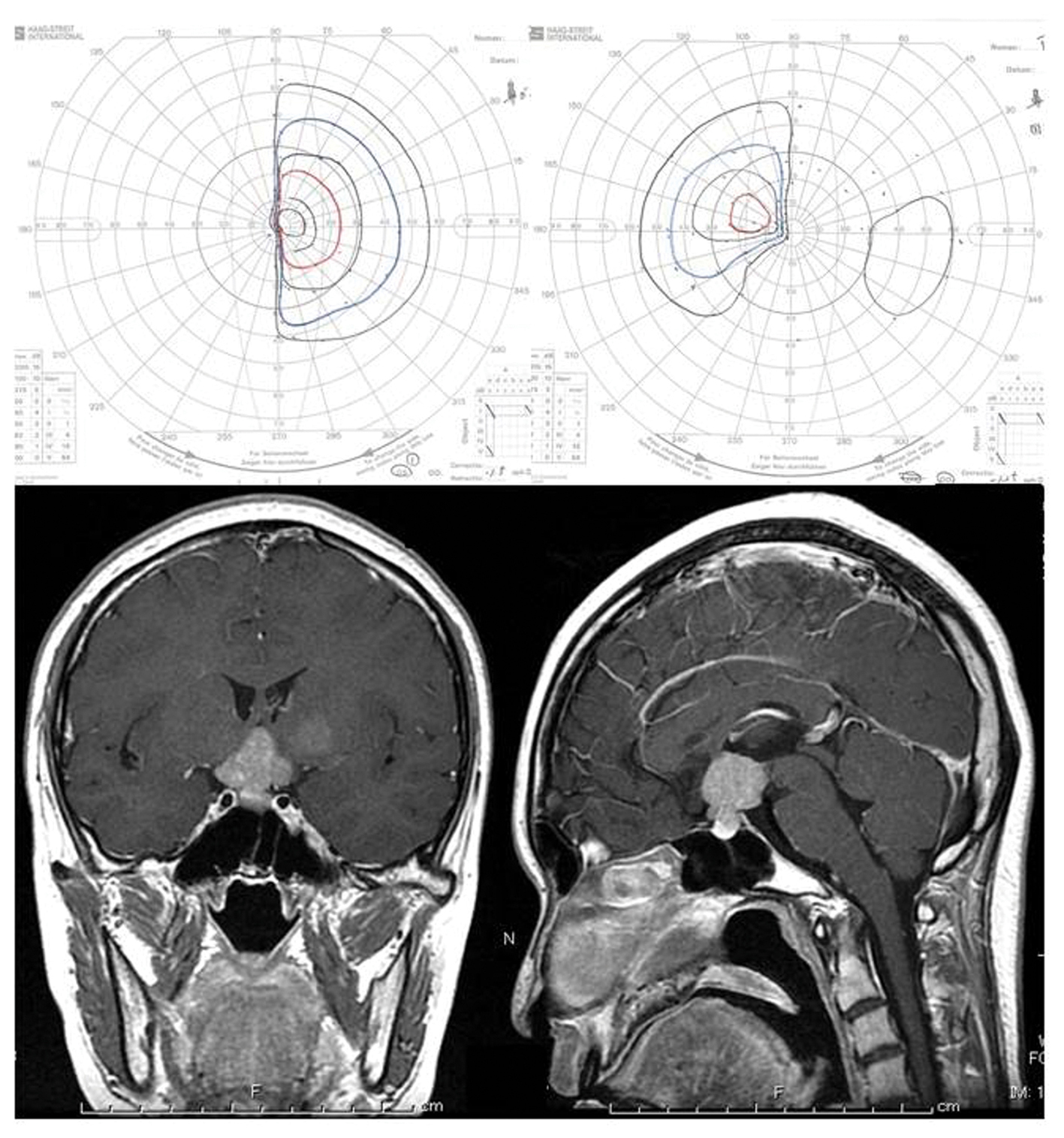
Figure 1. Upper: Goldmann perimeter reveals asymmetric bitemporal hemianopsia. Lower: Post-contrast MR imaging showed a contrast-enhanced sellar-suprasellar tumor and a light-enhanced lesion in the left basal ganglia.
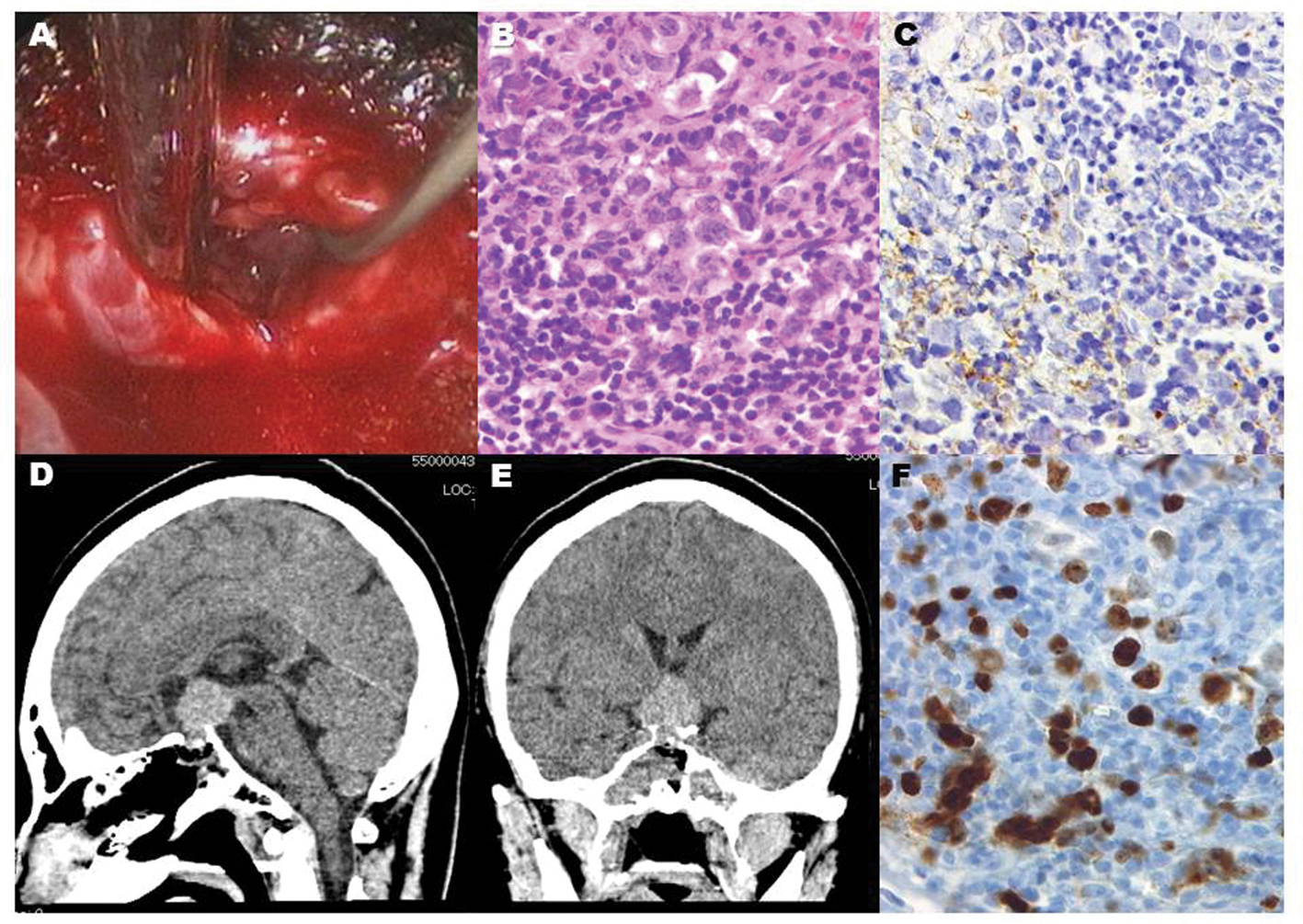
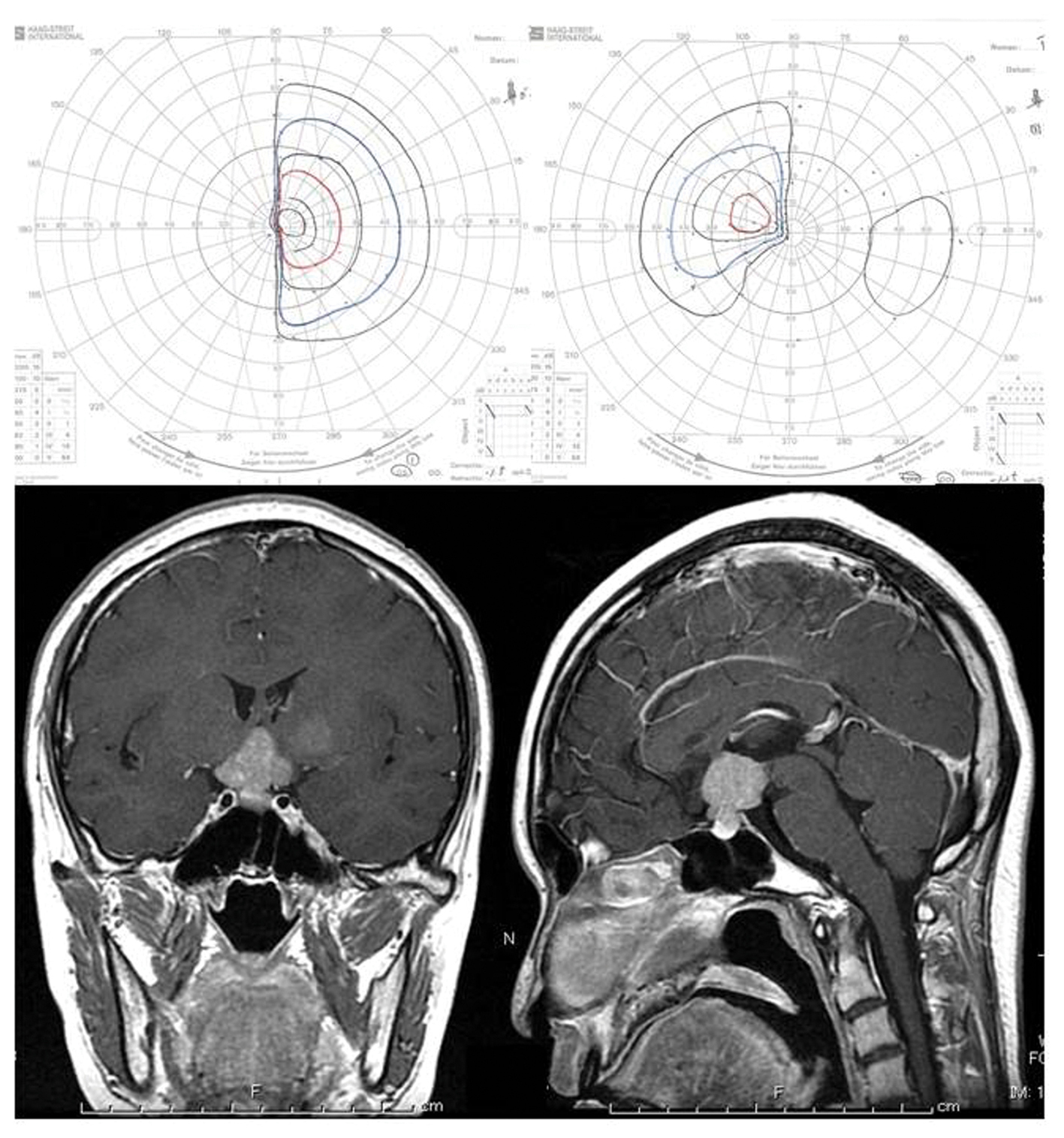
Figure 2. Endoscopic vision revealed grayish gelatinous tissue behind the thinned adenohypophysis (A). Histological diagnosis showed a biphasic population of mature lymphocytes and larger germinoma cells (B), staining of the cytoplasm and cytoplasmic membrane with placental alkaline phosphatase (C), and many MIB-1 positive cells (F), which are compatible with pure germinoma. Post-operative CT scans show that the intrasellar lesion was accessed by the endoscopic endonasal biopsy (D, E).
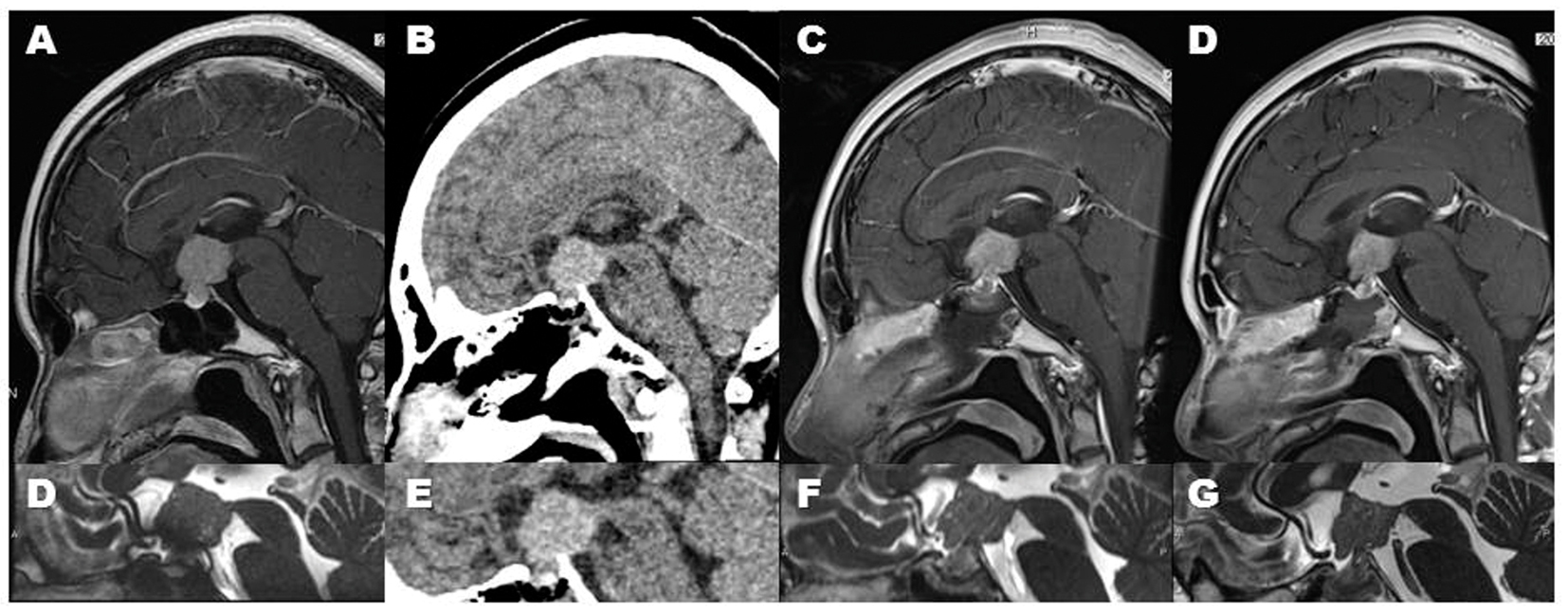
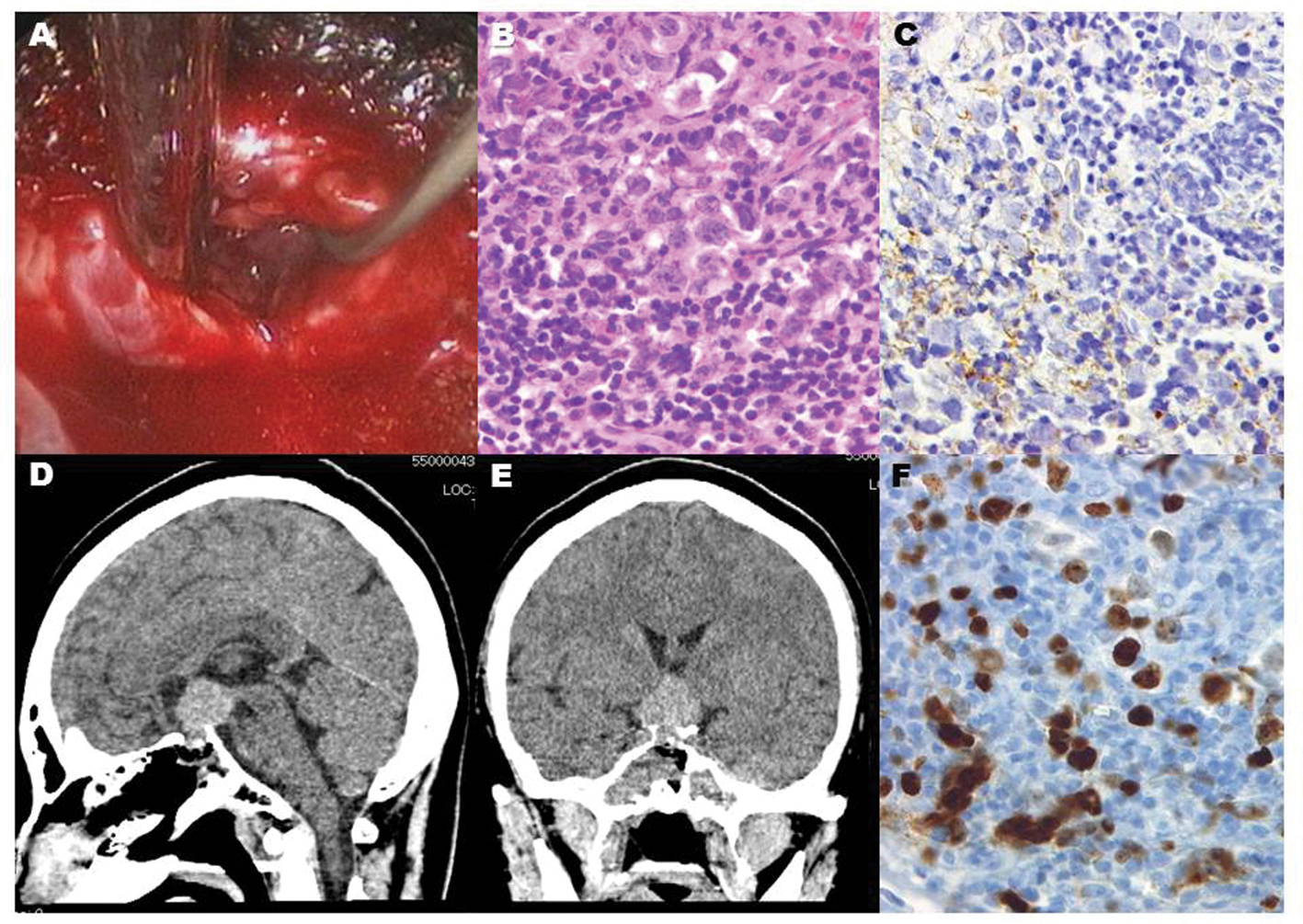
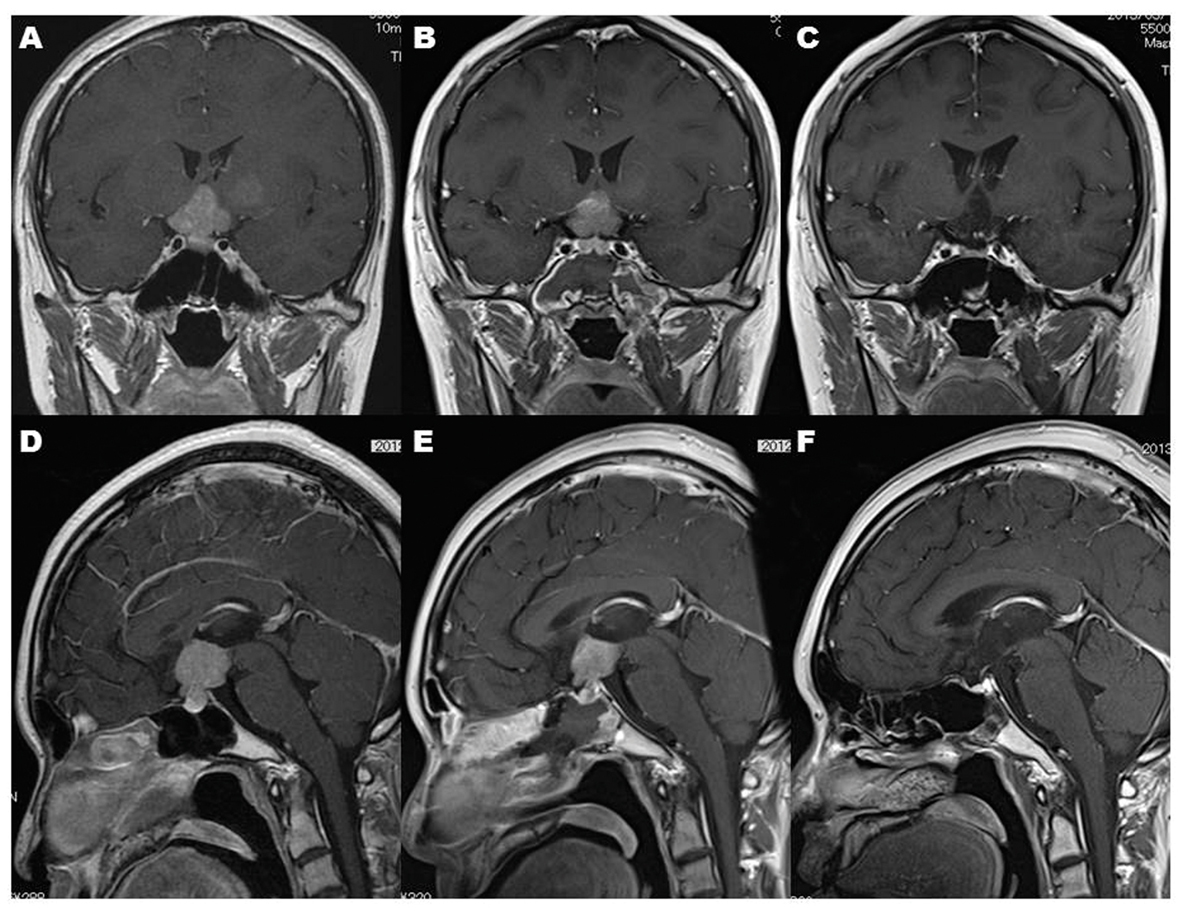
Figure 3. Serial images clearly demonstrated a regression of germinoma in this case. The regression was observed after the post-operative cranial computed tomography (CT) scan (B, E). Since this tumor is pure germinoma, this regression is compatible with diagnostic radiation-induced regression (DRIR). Sagittal MR images show the DRIR clearly: The tumor shows rapidly shrinking from the pre-CT-scanned state (A, D) through the third post-CT-scan day (C, F), to the eighth day (D, G).
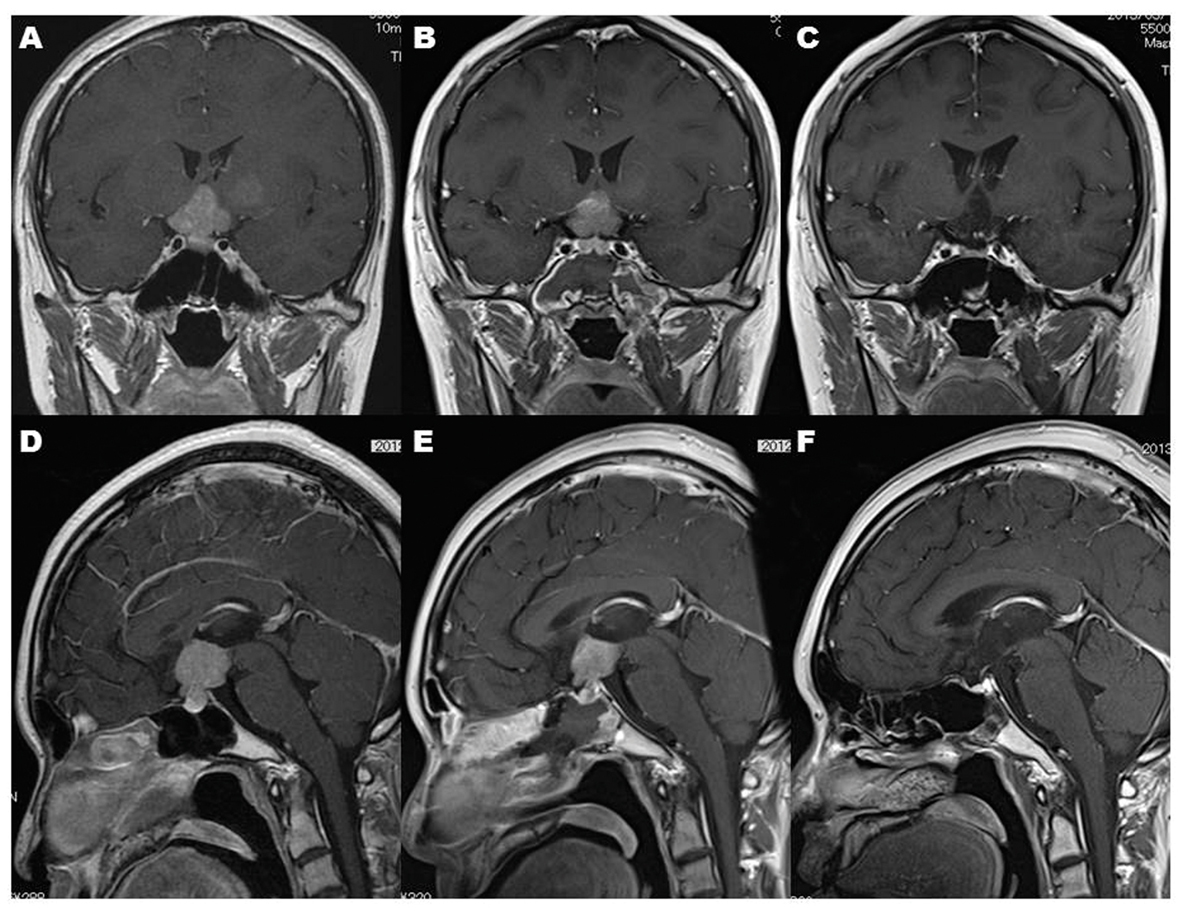
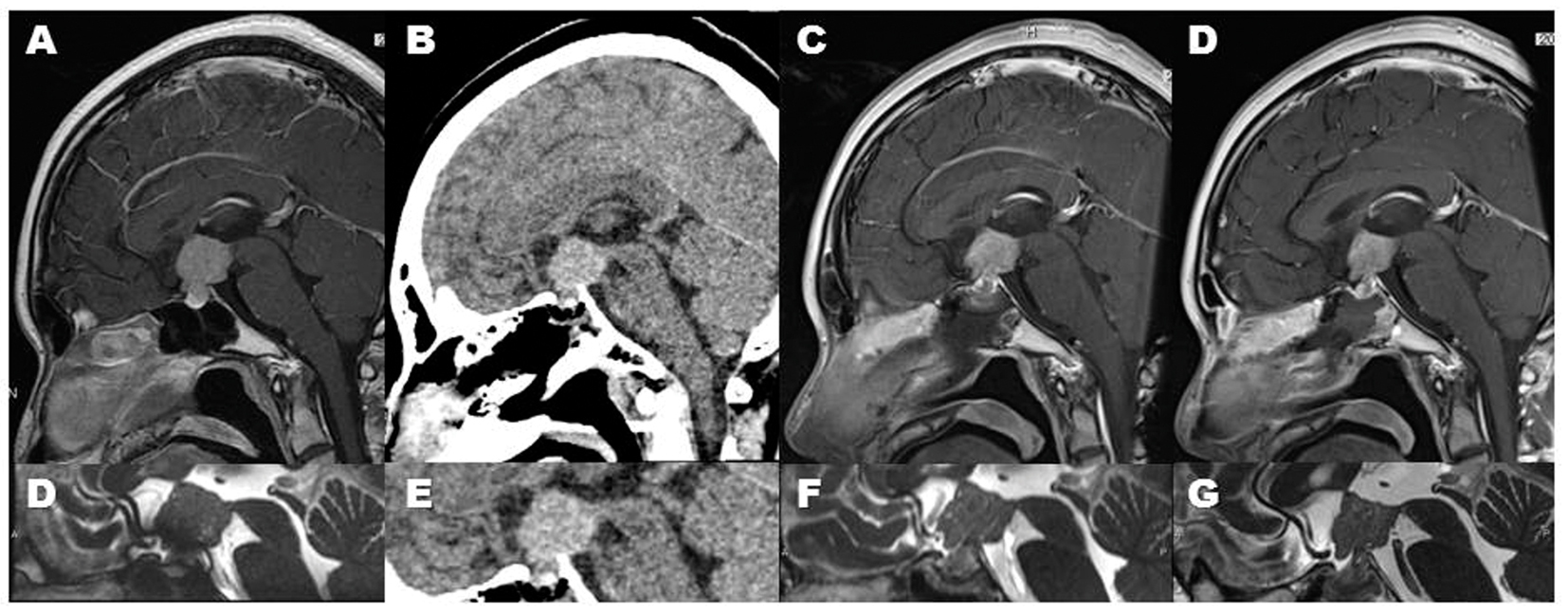
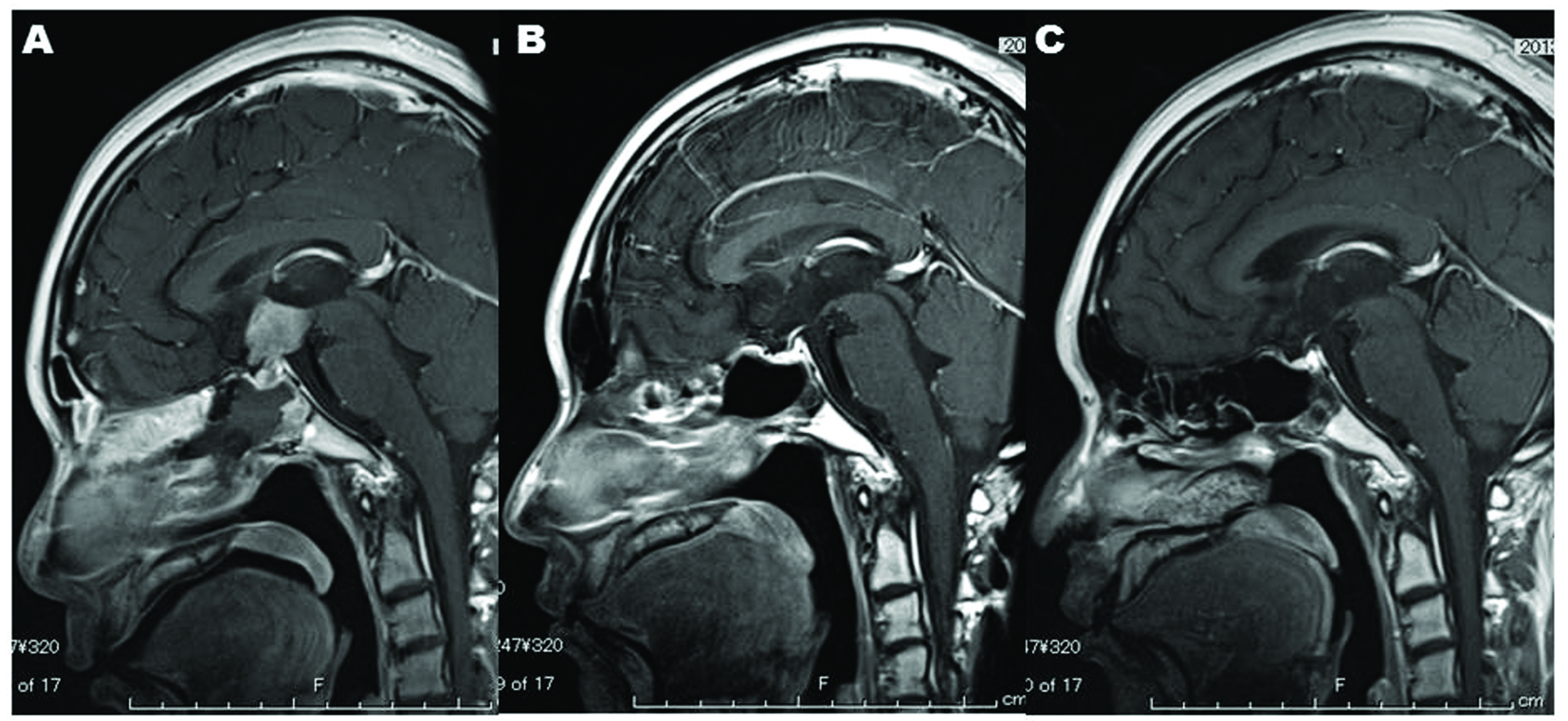
Figure 4. MR imaging demonstrates that the intracranial lesions before endonasal biopsy (A, D) and after endonasal biopsy (B, E) disappeared after completion of radiation therapy (C, F). Note that DRIR blurred the lesion of the left basal ganglia (A) after single cranial CT scan before radiation therapy (B).
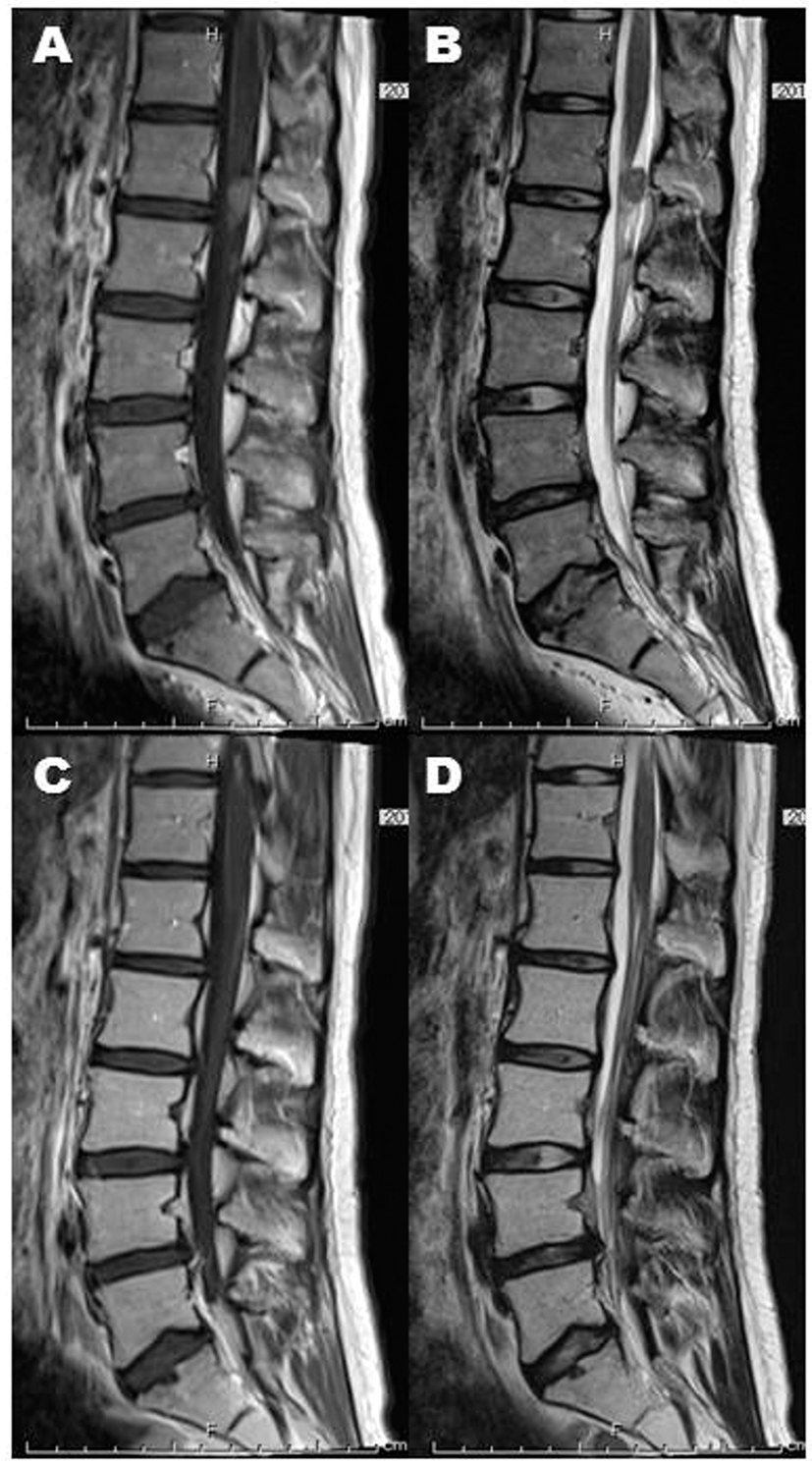
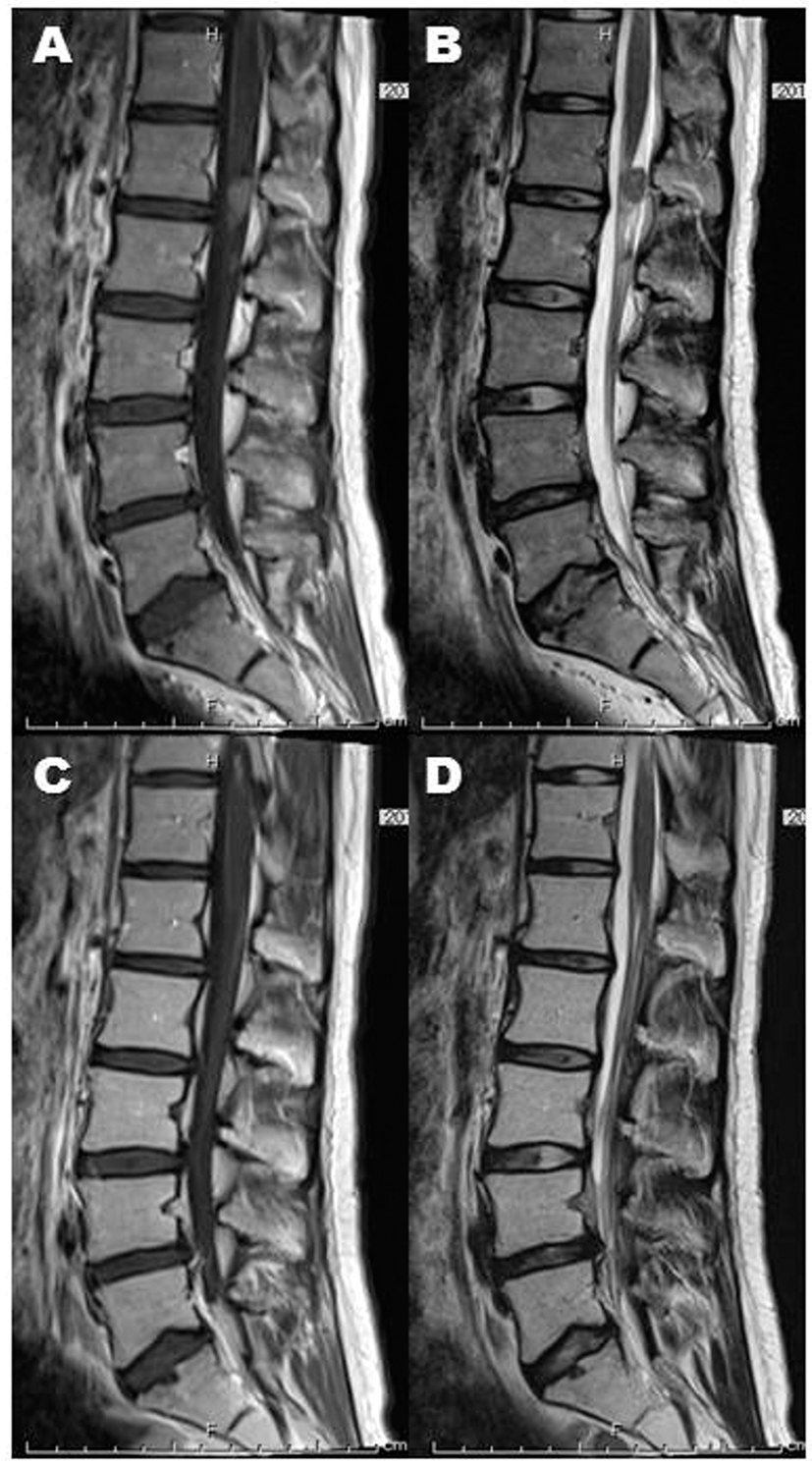
Figure 5. Spinal dissemination (A: post-contrasted sagittal image, B: T2-weighted sagittal image) also achieved complete remission (C: post-contrasted sagittal image, D: T2-weighted sagittal image).
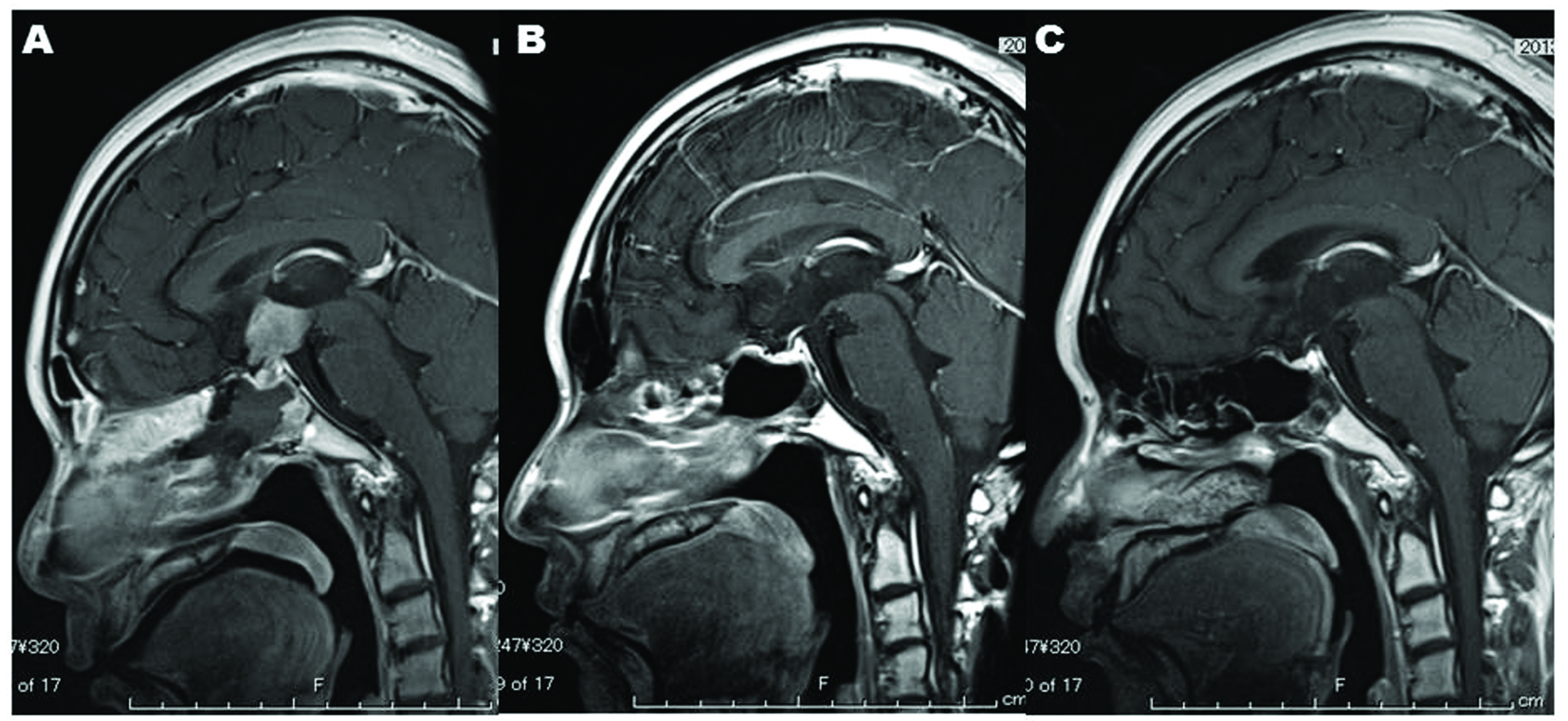
Figure 6. Nine months after completion of radiation, MR imaging shows no recurrence of the sellar-suprasellar lesion (C) and recovery of the intranasal and intrasphenoidal environments (C), which indicates that endoscopic endonasal biopsy is satisfactorily less-invasive.
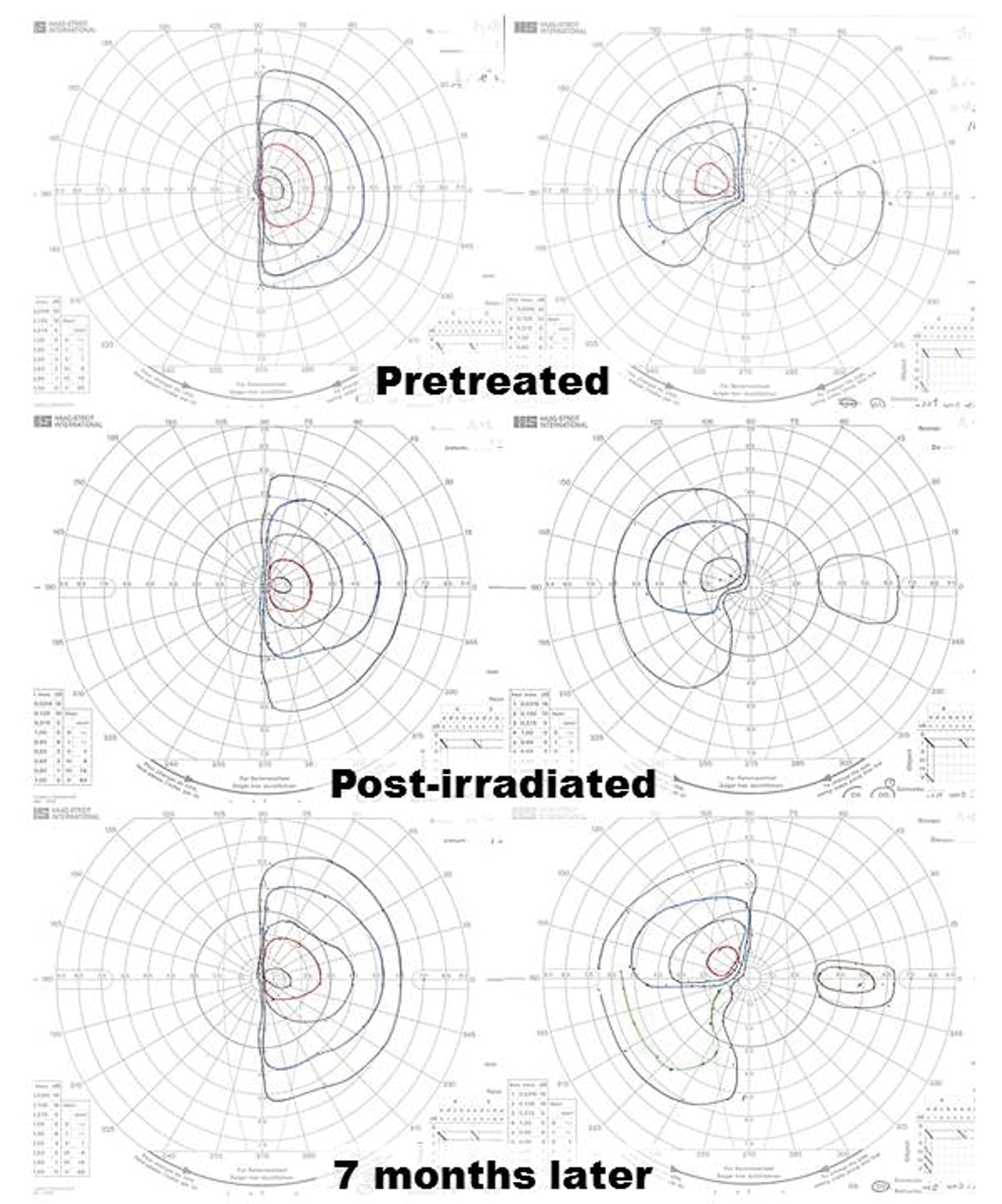
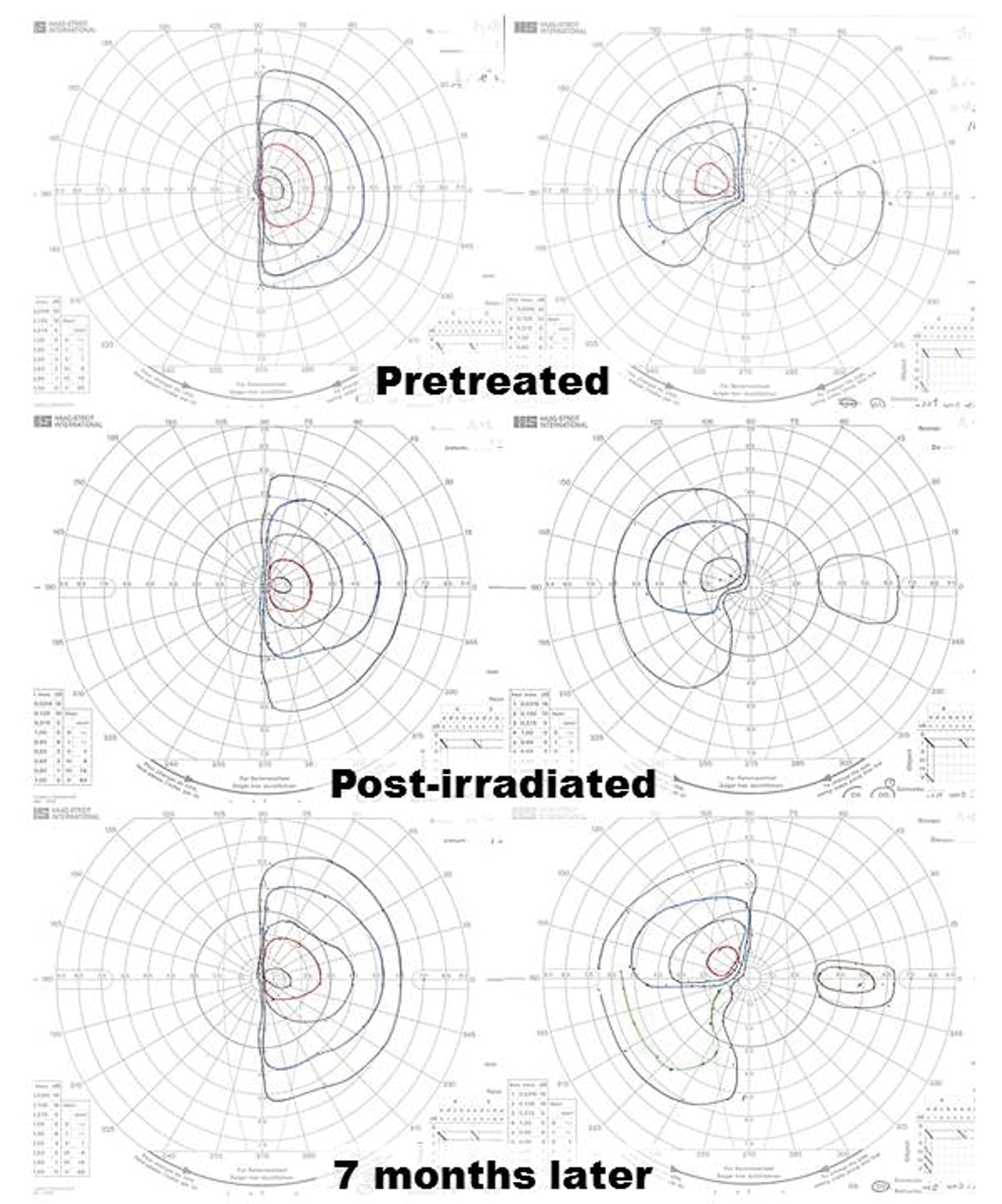
Figure 7. Despite complete remission of the lesion, restriction of the patient’s visual fields did not improve sufficiently. Goldmann perimeter revealed slight recovery of the left eye’s visual field 7 months after completion of radiation.
Tables
Table 1. Laboratory Data on Admission
| On admission | Reference | Unit |
|---|
| Growth hormone | 0.1 | < 2.5 | ng/mL |
| Prolactin | 62.0 | 2.7 - 28.8 | ng/mL |
| Luteinizing hormone | < 0.6 | | mIU/mL |
| Follicle-stimulating hormone | 1.2 | | mIU/mL |
| Thyroid-stimulating hormone | 2.28 | 0.6 - 4.1 | mIU/L |
| Free T3 | 1.9 | 2.1 - 3.8 | pg/mL |
| Free T4 | 0.5 | 0.9 - 1.6 | ng/dL |
| Cortisol | 1.0 | 3.5 - 18.3 | µg/dL |
| Estradiol | < 25 | | pg/mL |
| Somatomedin C | 44 | 161 - 425 | ng/mL |
| Na | 148 | 138 - 146 | mEq/L |
| K | 3.9 | 3.6 - 4.9 | mEq/L |
| Cl | 111 | 99 - 109 | mEq/L |
Table 2. Tumor Markers
| Before treatment | After treatment | References |
|---|
| hCG: human chorionic gonadotropin; PLAP: placental-like alkaline phosphatase. |
| Blood | | | |
| Alpha-fetoprotein (ng/mL) | 5 | 5 | < 6 |
| Beta-hCG (ng/mL) | 0.21 | < 0.1 | < 0.1 |
| Cerebrospinal fluid | | | |
| Beta-hCG (ng/mL) | 2.87 | < 0.1 | |
| PLAP (pg/mL) | 2116 | < 5 | |