| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Case Report
Volume 1, Number 4, October 2011, pages 168-169
A Rare Case of Chronic Alcoholism Related Marchiafava-Bignami Disease
Kanchana Seneviratnea, b, Sukran Altena, Mark Farrugiaa
aNewham University Hospital NHS Trust, London, UK
bCorresponding author: Kanchana Seneviratne
Manuscript accepted for publication September 5, 2011
Short title: Marchiafava Bignami Disease
doi: https://doi.org/10.4021/jnr57e
| Abstract | ▴Top |
Marchiafava Bignami disease (MBD) is a rare demyelinating disorder, mainly affecting the corpus callosum. This is a case of a 53 year old gentleman with chronic alcoholism who presents with neurological symptoms. Diagnosis is now much easier with MRI imaging. There have only been about 250 patients with MBD noted to be reported in the literature.
Keywords: Marchiafava-Bignami disease; Alcoholism; Diagnosis
| Introduction | ▴Top |
Marchiafava Bignami disease (MBD) is a rare demyelinating disorder, mainly affecting the corpus callosum. It was first described by two Italian pathologists: Ettore Machiafava and Amico Bignami. It is associated with chronic alcohol abuse. We present a case of this rare Marchiafava Bignami disease in a patient presenting as a fall.
| Case Report | ▴Top |
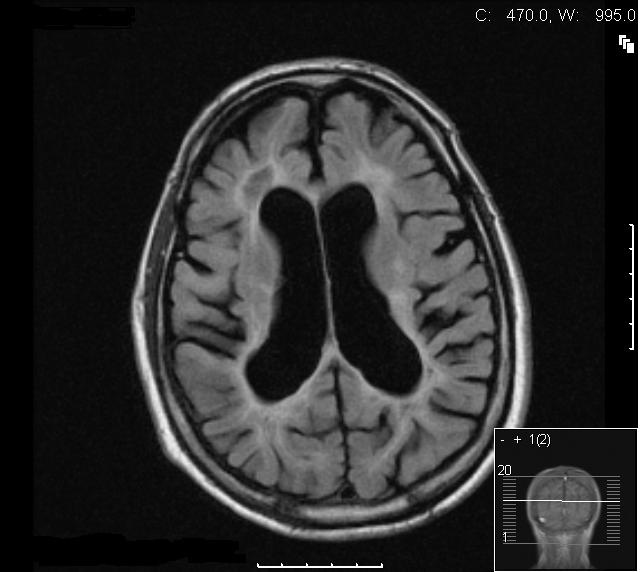
A 53-year-old Caucasian man with an alcohol consumption on average of 35 units per week, mainly lager, was admitted following a fall. On admission he appeared unkempt, confused, and had impaired memory. His carer expressed that he was usually confused and that he was likely to have been intoxicated before the fall. There was a one month history of unsteadiness on his feet. Physical examination revealed a malnourished individual and Mini-mental state examination showed short and long term memory deficits. On neurological examination there was reduced coordination, brisk reflexes in all limbs, an ataxic gait, dysdiadokokinesia, dysarthria and an intention tremor. Laboratory results revealed gamma glutamyl transpeptidase 60 (10-49), bilirubin 11 (5-21), alkaline phosphatise 277 (80-300), and alanine transaminase 38 (0-45). His tremors were initially assumed to be secondary to his alcohol withdrawal and were expected to reduce following the detoxification programme which was initiated. Despite the treatment however, the symptoms and signs of tremor, dysarthria and ataxia persisted. Magnetic resonance imaging (MRI) of his brain showed dilatation of the ventricles with cerebral atrophy. Confluent white matter signal abnormalities were present in the periventricular regions (Fig. 1, 2). In the posterior fossa and superior cerebellar vermis similar changes were noted and in the pons, areas of increased signal in the T2-weighted images were observed (Fig. 3, 4). One of the most striking abnormalities, however, was the demyelination of the corpus callosum. The presence of these findings suggested a diagnosis of Marchiafava Bignami. The patient was successfully weaned off alcohol following a detoxification programme with Pabrinex (Intravenous thiamine B1) and chlordiazepoxide. He was then treated with oral thiamine and vitamin B and discharged to a nursing home with improved gait and balance.
 Click for large image | Figure 1. Axial T2W section at level of the lateral ventricles showing moderately dilated symmetrical ventricles with extensive abnormal high signal in the periventricular and deep white matter. The cortical structures appear relatively normal. |
 Click for large image | Figure 2. Coronal T2W section at mid parietal level showing the extensive bilateral white matter abnormality consistent with acute demyelination. There is significant thinning of the body of the corpus callosum. |
 Click for large image | Figure 3. Axial STIR image showing extensive symmetrical periventricular and deep white matter signal abnormality consistent with acute demyelination. Note the generalised alcohol related atrophic changes. |
 Click for large image | Figure 4. T1W mid sagittal image showing the atrophy of the corpus callosum with altered signal within the corpus callosum indicative of demyelination and chronic changes. |
| Discussion | ▴Top |
The Italian pathologists Marchiafava and Bignami first described this disease following post-mortem brain analysis of three alcoholics (red wine drinkers) who presented with status epilepticus and coma in 1903. About 250 patients with MBD have been reported in several countries [1]. However it is felt that MBD goes under-reported and under-diagnosed and that its incidence is higher than that reported. This disease is due to demyelination of the corpus callosum and can also involve the cerebellar peduncles and putamen.
Diagnosis is made on the basis of clinical findings in combination with radiological imaging features. Diagnosis is now much easier with MRI imaging. The presenting features are non specific and include confusion, disorientation, psychotic and emotional symptoms, seizures, hemiparesis, dysarthria, ataxia, coma and death [2]. Most patients presenting with the acute type of MBD will go into coma and eventually die, although as in this case report, some survive.
In this case, the diagnosis was made on the basis of chronic alcohol abuse associated with the unresolving neurological symptoms and the MRI findings. The differential diagnosis in such a case would be Wernicke’s encephalopathy, Korsakoff syndrome and pontine myelinolysis. MRI imaging is most useful in differentiating MBD from the above differentials [3, 4]. The pathophysiology of MBD remains unclear. The involvement of the entire corpus callosum appears to be associated with a poorer neurological diagnosis. It is important to consider Marchiafava Bignami disease when non specific neurological symptoms with or without encephalopathy are present in an alcoholic. Early imaging with MRI should be considered in these cases.
| References | ▴Top |
- Shintani S and Shigaii T. Marchiafava Bignami disease with only slowly progressive cognitive impairment. Journal of rural medicine 2007; 1: 62-66.
- Arbelaez A, Pajon A, Castillo M. Acute Marchiafava-Bignami disease: MR findings in two patients. AJNR Am J Neuroradiol. 2003;24(10):1955-1957.
pubmed - Hlaihel C, Gonnaud PM, Champin S, Rousset H, Tran-Minh VA, Cotton F. Diffusion-weighted magnetic resonance imaging in Marchiafava-Bignami disease: follow-up studies. Neuroradiology. 2005;47(7):520-524.
pubmed doi - Gerlach A, Oehm E, Wattchow J, Ziyeh S, Glocker FX, Els T. Use of high-dose cortisone in a patient with Marchiafava-Bignami disease. J Neurol. 2003;250(6):758-760.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.







